Chapter Four
Treatment
Two kinds of treatment (therapy) of cardiac disease are generally recognized: (1) preventive (prophylactic) therapy , aimed at protecting a person from acquiring a disease or at halting the progress of existing disease, and (2) remedial therapy , aimed at abolishing or reducing symptoms or manifestations of a disease. Every intervention has to be considered from the standpoint of risk versus benefit to the patient. In this context risk is considered in a broad sense, including the possibility not only of death or worsening of health but also of unpleasant side effects or even undesirable changes in life-style.
The risk-benefit relationship applied to remedial therapy is clear-cut: every patient subjected to the risk of therapeutic intervention is expected to benefit from it; the implication is that if the goal of therapy is not attained, treatment is discontinued or changed. In preventive therapy the risk-benefit relationship is entirely different, because the benefit no longer can be gauged by the health of particular patients but rather is based on statistical probability. Many subjects are exposed to the risk—if there is any—but only a few are expected to benefit from the therapy. Consider these two examples. (1) If a certain population elects to modify its diet in the hope of reducing the probability of future heart attacks, the benefit cannot be measured; the risk, however, consists only of a voluntary change in life-style. (2) If anticoagulants are administered to patients who are known to be prone to form clots in the heart, in order to reduce the risk of a stroke, the drug introduces a different risk, though admittedly remote—that of a serious hemorrhage. Assume that for a certain group of cases the risk of stroke can be
reduced by half—say, from one chance in 50 to one chance in 100. For each 100 patients, one will be spared the stroke—99 are subjected to risk of hemorrhage without expected benefit. Here a thoughtful consideration of the risk-benefit relationship is needed to decide in each case whether such treatment should be initiated.
Preventive cardiology is playing an increasingly important role in managing heart disease. Two types of prevention can be distinguished: (1) primary prevention , aimed at protecting a healthy person from developing a cardiac disease, and (2) secondary prevention , aimed at keeping disease already established in a patient from progressing or from leading to complications. The same type of intervention may be applied to primary and secondary prophylactic therapy. For example, institution of a low-fat, low-cholesterol diet is considered primary prevention, if applied to the general population, or secondary prevention, if applied to patients who have recovered from coronary heart attacks.
General Management of the
Cardiac Patient
The majority of patients suffering from cardiac disease are afflicted by a chronic, often lifelong problem. Consequently, their medical management goes beyond conventional treatment and involves recommendations concerning life-style. Patients with milder varieties of heart disease are often permitted to lead a normal, totally unrestricted life, except for such minor interventions as administering an antibiotic drug before dental extractions as a precaution against infection. Children with heart disease may require specific instructions concerning physical education and recreational activities as well as vocational guidance. Patients whose disease have progressed to a point of some disability may need a detailed program regulating their activities and diet and may be counseled regarding some occupational and environmental factors.
The most detailed set of regulations applies to patients recovering from heart operations or from an acute myocardial infarction. Here a specially trained team may take charge of cardiac rehabilitation. The goal is to guide and facilitate the transition from acute hospital care to as normal a life as possible, while emphasizing secondary prevention of further heart damage. Cardiac rehabilitation is usually divided
into three stages: stage 1 involves in-hospital treatment; stage 2, immediate convalescence; and stage 3, long-term support. During the first stage the patient is guided toward resuming activities at a gradual pace often by physical therapists and occupational therapists, in combination with psychological support. On leaving the hospital, the patient usually receives individual instruction regarding an exercise program, based on treadmill tests, as well as other advice regarding life-style. Exercise is often performed in organized rehabilitation units under medical supervision. The third stage is important for those patients who have some residual disability and may benefit from constant supervision.
Cardiac Drugs
Many drugs for the treatment of heart disease are now available, and the number is constantly increasing. Drugs are strictly regulated: new drugs can be placed on the market only after approval, following a series of tests, by the Food and Drug Administration. Three features of every drug are evaluated: (1) efficacy, (2) side effects, and (3) toxicity.
To demonstrate the effectiveness of a cardiac drug, controlled studies have to be performed. Typically its action is compared with that of a placebo, tablets similar in appearance to the drug but containing an inert substance, such as sugar. Inasmuch as responses to drugs vary from person to person, and some patients may even show improvement when taking the placebo (owing to psychological influences), large numbers of observations are often needed to demonstrate that a drug has the predicted effect on heart disease.
Side effects consist of undesirable consequences of taking a drug that may develop while the drug is administered in the recommended dose and exerting the desired effect on disease. Among common side effects of cardiac drugs are nausea, diarrhea, sleepiness, and reduced sexual drive.
Drug toxicity refers to serious, even fatal consequences of administering a drug. There are two mechanisms of drug toxicity: (1) toxic effect caused by a dosage that is too high for a given patient; and (2) toxic effect caused in certain patients who have or develop hypersensitivity to a certain drug even though it is being administered in the recommended dosage. Hypersensitivity to a drug often involves
allergic reactions that may become progressively more severe as treatment with the drug continues or when treatment is repeated. Some of these reactions may be life-threatening.
Frequently treatment of a cardiac condition requires the administration of more than one drug. In that case it is necessary to take into consideration the relationship of drugs to each other, or drug interaction . In many instances two drugs have no such relationship: each drug exerts its effect independently of the other. However, drug interaction is common and may take place in a variety of ways:
Two drugs may facilitate each other's action, so that smaller doses of each may attain the desired effect with better tolerance and lower potential for toxicity (synergistic action).
Two drugs may reduce each other's potency, making higher doses necessary to produce the desired effect (antagonistic action).
The addition of a second drug may alter the action of the first drug, which may previously have been effective and well tolerated: the new drug may make the first drug toxic in some instances or simply ineffective in others.
Drug interactions are of considerable importance in patients requiring treatment by multiple drugs, and caution is required in selecting compatible drugs and regulating dosages.
Drugs are foreign substances the body tries to destroy or excrete. Different drugs are handled in different ways: some are eliminated with the urine or feces, some are destroyed by one of the organs (usually the liver), and some are changed into inert substances. The length of time it takes to eliminate an active drug plays a role in the way the drug is administered. Most drugs are absorbed from the gastrointestinal tract into the bloodstream, where their level can be measured. Blood level of a drug decreases at a fixed rate for each drug. The time required to halve drug content in the blood from its initial level is called the half-life of a drug, and it helps in determining how often a given drug has to be taken by the patient. Most cardiac drugs have half-lives of a few hours and hence must be administered at least three times a day. Those with a long half-life need to be taken only once daily.
The standard method for administering cardiac drugs is in the form of tablets or capsules. Liquid medicines are rarely used. However,
for a variety of reasons drugs may have to enter the body by other than the oral route, or parenterally . Parenteral drug administration involves injecting the drug underneath the skin (subcutaneous), into a muscle (intramuscular), or into a vein (intravenous). A drug may be administered parenterally either because it acts faster thus administered than when given orally or because it would be destroyed by digestive juices.
In acutely ill patients parenteral administration of drugs is preferred. In such cases the most common means is continuous intravenous drip. The drug is dissolved in a solution of salt or glucose, and a measured amount enters the body, maintaining a steady level of the drug. By regulating the speed of the drip, the effect of the drug can be increased or decreased as the need arises. Other parenteral modes of administering drugs include sublingual (some drugs, such as nitroglycerin, take effect rapidly when dissolved under the tongue) and transdermal (some drugs can be absorbed through the intact skin as an ointment or on specially designed patches).
Drugs used specifically in the treatment of heart disease are categorized according to their pharmacological effects. Some drugs have multiple actions and are used for different purposes, such as for treatment of high blood pressure and of heart failure. In most categories there are several drugs with almost identical effects. Commonly used cardiac drugs can be grouped in two ways. The first is according to physiological action:
Drugs enhancing the force of cardiac contraction . The classic drug, digitalis, is derived from the foxglove plant and has been in continuous use for more than two hundred years. A few newer drugs are now available, predominantly for short-term treatment.
Diuretics . This widely administered group of drugs is used to counter fluid retention caused by heart failure and to treat hypertension.
Beta-adrenergic blocking agents . These drugs are capable of blocking one of the functions of the autonomic nervous system. The prototype of a drug in this category is propranolol, first developed in the 1960s. There are multiple uses of these drugs in heart disease—to reduce high blood pressure, to reduce or eliminate attacks of angina pectoris, to reduce or prevent certain arrhythmias, and to slow the heart rate.
Calcium channel blocking agents . These drugs relieve or prevent spasm of blood vessels (particularly the coronary arteries), reducing high blood pressure, and reducing or eliminating attacks of angina pectoris. In addition, several of these drugs have antiarrhythmic properties.
The second grouping is according to therapeutic effect:
Antiarrhythmic drugs . Drugs aimed at the prevention or elimination of arrhythmias include some drugs in the categories mentioned above. Quinidine and procainamide are the prototypes and other powerful antiarrhythmic drugs have been introduced, some of them highly toxic but uniquely effective in life-threatening arrhythmias.
Anti-heart failure drugs . Besides diuretics and drugs enhancing the force of cardiac contraction, these include vasodilator drugs that reduce the heart's workload and mitral regurgitation.
Antihypertensive drugs . Several categories of drugs have the property of reducing blood pressure, by various mechanisms. Treatment of hypertension thus often involves the use of more than one drug, which together may act synergistically.
Antithrombotic drugs . The problem of clot formation within the heart or the blood vessels is addressed by three types of drugs. (1) Thrombolytic drugs, capable of dissolving existing clots. (2) Drugs inhibiting aggregation of platelets in the blood, such as aspirin, are used prophylactically. (3) Anticoagulant drugs are a more effective means of clot prevention. However, they carry a risk of bleeding and require periodic tests of their effectiveness.
Antianginal drugs . Nitrates (nitroglycerin and long-acting derivatives of it) dilate the coronary arteries. Other drugs include beta-adrenergic and calcium channel blocking agents, both of which act by reducing the requirements of the heart for oxygen.
Lipid-lowering drugs . These help reduce atherosclerosis by lowering the blood levels of cholesterol and triglyceride.
Drugs administered for remedial purposes need monitoring. In some cases the effects are obvious to the physician or patient. For instance, diuretics cause the patient to pass large quantities of
urine, and their effects can be measured by recording daily body weight. Antihypertensive drugs require frequent measurement of the blood pressure, which often can be done by the patient. The effectiveness of antianginal drugs is determined by the patient's observation regarding the number and severity of attacks of angina. In such cases the dosage of a drug and suitability of a particular therapy can be directly determined. Measurement of the blood content of some drugs may provide guidance in regulating dosages.
The effectiveness of drugs administered prophylactically cannot be evaluated directly. In some cases tests are available to help establish the dosage of a drug (for example, the prothrombin time test for anticoagulants) or to determine effectiveness (such as serum cholesterol level in the evaluation of cholesterol-reducing diets or drugs). If no tests are available to determine the safety of a prophylactic drug, a standard dosage is prescribed and maintained, provided no side effects develop.
Drug toxicity often presents serious problems. Immediate reactions in patients to a new drug can usually be controlled by reducing dosage or substituting a similarly acting drug. However, some cardiac drugs produce toxic reactions only after weeks or months of apparently successful treatment; furthermore, the toxic effect may not be apparent. Among such slowly appearing toxic effects are drug-induced reduction in white blood cells or platelets in the patient's blood, liver damage, development of cataracts, changes in personality, and depression. Some drugs have been suspected of being carcinogenic.
As stated, the potential toxicity of many cardiac drugs requires thoughtful consideration of the risks and benefits, especially in cases where a drug must be administered for long periods or permanently. Careful clinical observation and the performance of periodic blood and liver function tests may sometimes aid in detecting drug toxicity. Nevertheless, in certain life-threatening conditions, such as ventricular arrhythmias, the risk of serious toxic reaction is acceptable as a lesser evil.
Interventional Cardiac Therapy
Traditionally treatment of heart disease fit into two classes, medical and surgical. Now a third mode of treatment is available and widely
used, intermediate between medical and surgical—interventional therapy , performed by specially trained cardiologists rather than cardiovascular surgeons. Some of these procedures represent alternatives to surgery; in selected cases they may be equally effective yet simpler and less expensive and require the patient to spend much less time in recovery. Others have specific uses and indications. Among such procedures are
balloon coronary angioplasty (percutaneous transluminal coronary angioplasty, or PTCA)
balloon valvuloplasty
temporary or permanent use of pacemakers
intraaortic balloon pump
interventional treatment of arrhythmias
Coronary angioplasty was developed in the late 1970s, and it has proven successful in relieving stenosis of the larger branches of the coronary arteries. Atherosclerosis of arteries produces plaques that reduce the amount of blood the artery is able to deliver to the affected organ. When such plaques significantly reduce the lumen of a coronary artery and are accessible, as demonstrated by coronary arteriography, angioplasty is performed by introducing a specially designed cardiac catheter into the arterial system. At one end of the catheter is a balloon, which when deflated fits snugly around the catheter; a separate channel connects it with the end of the catheter outside the body, through which it can be inflated. The inflated balloon has a long, cylindrical shape of fixed diameter, which can widen the tip of the catheter considerably, filling the inside of the artery. Under fluoroscopic examination the tip of the catheter is placed in the portion of the coronary artery narrowed by the plaque. The balloon is then inflated with a liquid at controlled and measurable pressure, compressing the plaque and thereby greatly reducing the stenosis (fig. 19). Cutting devices, lasers, and small framework-like devices called stents can be used in difficult cases.
The success of coronary angioplasty in improving blood supply to the heart by relieving obstruction in a coronary artery encouraged the development of a similar technique to relieve valvular narrowing. Balloon valvuloplasty works on the same principle as PTCA;
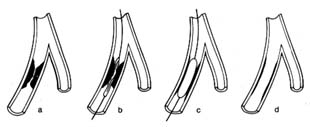
Figure 19. Coronary angioplasty. (a) Coronary branch showing severe stenosis.
(b) Catheter placed in this branch with a deflated balloon at the level of the stenosis.
(c) Inflated balloon compressing the stenosing plaques.
(d) Minimal residual stenosis after the removal of the catheter.
the catheters and balloons are appropriately larger, and they differ in design. The catheter tip with deflated balloon is placed at the stenosed valve, which widens when the balloon is inflated.
Electronic pacemakers have been in use since the 1960s. They were introduced to provide protection from sudden death caused by failure of the natural pacemaker. The artificial pacemaker consists of a generator that rhythmically discharges electrical impulses. It is connected with an insulated wire inserted through the patient's venous system, so that its exposed tip is in contact with the muscle of the right ventricle or right atrium or both. The pacemaker has two functions: pacing , i.e. generating rhythmic electrical impulses, and sensing , i.e. detecting electrical impulses from the beating heart, which inhibit the artificial impulses from the generator. The sensing function permits the pacemaker to become active only when needed, assuming a standby function in patients who develop temporarily excessive slowing of the heart, or "pauses" (chap. 6). In patients with permanently slow heart rhythm the electronic pacemaker operates at all times. The point of stimulation of the heart is selected in accordance with the type of bradycardia (abnormally slow heartbeat): in diseases of the sinus node the atrium is stimulated; in complete heart block, the ventricle.
The pacemaker can be set up as a temporary measure, with the stimulating wire inside a cardiac chamber connected to a generator located outside the body. More often, however, pacing is permanent, in which case a miniaturized generator is placed under the skin in a small pocket made by surgical incision, usually underneath the collarbone. In permanent pacemakers the generator
imbedded under the skin can be programmed from outside the body to adjust the heart rate.
Pacing has now become quite sophisticated. The most important development has been the dual-chamber pacemaker . Separate wires are introduced into the atrium and the ventricle. The generator can sense and initiate pacing of the atrium, if that chamber fails to receive the normal stimulus, or the ventricle, if the atrial impulse fails to reach the ventricle. Furthermore, if needed, both chambers can be sequentially paced, maintaining the natural interval between them.
Intraaortic balloon pumps act as boosters supporting the pumping action of a failing left ventricle. Inasmuch as such devices can safely be used for no more than a few days, this method of treatment is intended only to tide over a temporary malfunction of the left ventricle. A specially designed catheter is introduced into an artery in the groin and advanced into the descending aorta. The catheter is surrounded by an inflatable balloon along most of its length. The deflated balloon is connected to a pump (outside the body), which is synchronized with the heart action by means of signals coming from an electrocardiogram. During cardiac systole the balloon remains deflated; during diastole, when the aortic valves are closed, the pump inflates the balloon, which fills the inside of the aorta, thereby acting as a pump and displacing the blood (fig. 20). By this means the blood flow into the critical areas—the brain and the coronary circulation—receives an additional boost in diastole, supplementing the normal pumping action of the heart in systole; furthermore, this technique helps maintain blood pressure at an adequate level. The principal use of the intraaortic balloon pump is in the treatment of shock, particularly when it is caused by failure of a cardiac ventricle; it is also used in treating unstable angina pectoris (chap. 7) and in stabilizing some patients after open-heart surgery.
Interventional treatment of arrhythmias includes the following techniques:
external defibrillation of the heart in cardiac arrest
termination of tachycardias by electric shock (cardioversion) or by means of pacemakers
deliberate induction of damage to the conducting system of the heart by means of special catheters to control certain life-threatening arrhythmias
Ventricular fibrillation , uncoordinated twitching of the heart muscle, is the commonest cause of cardiac arrest. The heart ceases to pump blood, effectively, and the condition is fatal unless it can be reversed within four to five minutes. External defibrillation , application of electric current to the outside of the chest in the region of the heart by means of two conductive paddles, may restore normal heartbeat—the essential step in cardiac resuscitation.
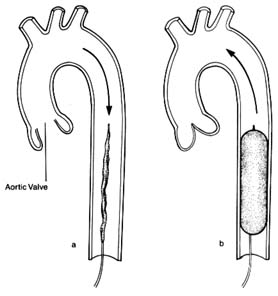
Figure 20. Intraaortic balloon pump. A deflated balloon is placed in the descending
aorta and is connected with a pump, the action of which is synchronized with
cardiac contraction and relaxation by means of an electrocardiographic signal.
(a) During ventricular systole (open aortic valve) the balloon remains deflated
and blood flow is normal. (b) During ventricular diastole (closed aortic valve)
the balloon is inflated and displaces the blood in the descending aorta.
A related technique is used to restore a normal heart rhythm in certain arrhythmias involving tachycardia , abnormally rapid heart action. Here, however, the electric shock has to be delivered at a specific point in the cardiac cycle and must be synchronized by an electrocardiographic signal. This procedure, cardioversion , may be applied in emergencies for acute arrhythmias or electively for chronic arrhythmias. Whereas in cardiac arrest defibrillation is performed on unconscious patients, candidates for cardioversion, a very painful procedure, are conscious and hence have to be put under general anesthesia or heavy sedation.
A new application of the technique of treating arrhythmias electrically is the implantable defibrillator and cardioverter , which has been approved for limited use. At present this apparatus has to be inserted surgically, its wires sutured to the surface of the heart and its generator implanted under the skin. The objective of this method is to defibrillate automatically patients who develop ventricular fibrillation or to cardiovert ventricular tachycardia, thus preventing cardiac arrest. The generator is programmed to sense and diagnose ventricular fibrillation or ventricular tachycardia and to administer an appropriate electric shock to restore regular rhythm. The treatment is indicated only in patients with a clearly demonstrated high risk of fatal arrhythmia.
Certain tachycardias can be terminated by delivering rapid impulses by means of an electronic pacemaker placed temporarily with its tip in the right atrium. This method, pacing overdrive , is an alternative to cardioversion; it has the advantage of being painless, thus obviating the need for anesthesia.
A new method of treatment of certain serious arrhythmias originating in the atrium is now being developed and tested. Certain atrial arrhythmias occurring periodically may cause serious disability and be unresponsive to drug therapy. It is possible, by manipulating a specially designed catheter, to destroy the tract conducting impulses from the atria to the ventricles (the atrioventricular node or bundle of His), thereby shielding the ventricles from the rapid stimulation. Certain abnormal pathways can be destroyed while preserving the normal pathways. In some cases permanent pacemakers may be necessary after such an ablation procedure. Obviously, such a drastic step should be taken only if other means of controlling the heart fail.
Surgical Therapy
The development of heart surgery constitutes one of the most dramatic advances in the health field in this century. During most surgery on the heart today the pumping and oxygenating of the blood is done outside the body by a heart-lung machine. Few operations—resection of the pericardium, closed mitral valvotomy—can be performed on a beating heart with the blood circulating normally. Cardiopulmonary bypass is obligatory in open-heart surgery. There are four requirements for the performance of open-heart surgery: (1) the blood has to be pumped and oxygenated outside the body; (2) the heart cavities have to be empty; (3) the heart motion has to be stopped; (4) when the circulation and heart motion are restarted, the function of the ventricles has to be restored to its preoperative level.
When open-heart surgery was first developed in the 1950s, the task of fulfilling these requirements was indeed formidable. The pump-oxygenator was a highly complex apparatus; several units of blood were needed to start the procedure; and the rate of complications from the artificial perfusion alone was considerable. Since then technology has greatly simplified cardiopulmonary bypass. A simple pump-oxygenator services blood circulating outside the body in disposable tubes and containers (fig. 21). The heart is stopped by injecting into it a solution containing a combination of electrolytes (potassium is a major component). In addition, the heart is cooled so as to reduce its oxygen requirements (hypothermia). Present techniques attain almost perfect preservation of heart muscle function. Cardiopulmonary bypass surgery lasts from one to twelve hours, with some increase in risk in the longer operations. Although surgical results are usually related to the skill and experience of the cardiovascular surgeon, the overall success of the operation is greatly influenced by the contributions of the entire cardiac surgical team of physicians, nurses, and technicians, whose responsibility is to prepare the patient for surgery, administer general anesthesia, supervise the perfusion of blood during cardiopulmonary bypass, and attend to postoperative care.
The overall risk of heart operations varies widely. Several studies have shown that institutions performing a high number of operations are likely to have lower surgical mortality than other institutions.
Commonly performed heart operations include coronary bypass
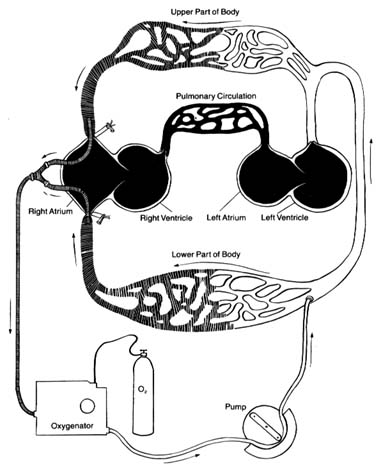
Figure 21. The artificial circulation used during open-heart surgery (cardiopulmonary bypass,
using a heart-lung machine). Venous (deoxygenated) blood is shown by shaded areas,
oxygenated blood by white areas. Sections of the circulation shown in black represent the
areas bypassed by the artificial circuit and void of blood, which can be opened for repair.
All the blood returning from the superior and inferior venae cavae is drained and channeled
through an oxygenator to be pumped into the arterial system. The blood is prevented
from reentering the heart by the closed aortic valve.
surgery, repair or replacement of heart valves, and correction of congenital malformations of the heart. Coronary bypass is now the most frequently performed major operation in the United States. Even though it does not require opening the heart chambers, the delicate suturing of the arteries has to be performed on a still heart.
Cardiac transplantation has now become a common operation. Its introduction in 1967 was followed by disillusionment because of the low survival rate. However, the development of effective drugs preventing rejection of the transplanted heart has successfully established this procedure, with the majority of patients surviving at least five years. The surgery itself is relatively simple, but the complexity of the overall subsequent care of transplant recipients limits its performance to a small number of institutions. Furthermore, the number of candidates for cardiac transplantation far exceeds the number of suitable donor hearts.
The artificial heart was widely publicized in the media in the mid-1980s when it was implanted into a few patients. Yet the dismal results and astronomical costs made it totally impractical. Some experts doubt whether it will ever become a viable form of treatment. However, a simple mechanical pump assuming the function of one or both ventricles has been used with some success as a temporary bridge when the heart fails totally, until a donor for cardiac transplantation becomes available.