Sequelae of Coronary Atherosclerosis
Coronary-artery disease is related to a single consequence of atherosclerotic reduction of coronary blood flow—ischemia of the heart muscle. Myocardial ischemia is a decreased delivery of oxygen to heart muscle cells such that myocardial oxygen demand exceeds the supply of oxygen through the coronary circulation. Thus ischemia may develop if myocardial oxygen requirements increase but supply remains the same or if such requirements remain stable but blood flow supplying oxygen is reduced. Increased myocardial oxygen demand is related to cardiac workload. For example, exercise steeply increases the oxygen requirements of the heart muscle; a similar effect, though less pronounced, is produced by factors elevating arterial pressure.
To explain the relationship between oxygen supply and demand, we need to understand the concept of coronary reserve . Approximately 20 percent of the maximum capacity of the coronary arteries to supply the heart muscle with oxygen is required by a person at rest. The remaining 80 percent of potential blood flow represents the coronary reserve available to take care of increased cardiac oxygen demands. An atherosclerotic plaque may grow to the point where coronary blood flow is affected, reducing the coronary reserve from 80 percent to 60 percent. In this case myocardial ischemia would develop only when the full reserve was required, such as during strenuous exercise, at which time the person would experience chest pain. Further growth of a plaque eliminates more cardiac reserve, producing chest pain with less-strenuous activity. More-severe stenosis may reduce coronary reserve to the point where relatively light activity produces ischemia. Myocardial ischemia (and its accompanying chest pain) may also result from other factors raising myocardial oxygen demands, such as increases in blood pressure or heart rate due to stress or excitement. Ischemia
caused by increased myocardial oxygen demands is by definition reversible, for adequate oxygen supply resumes as soon as oxygen requirements return to normal (basal) levels.
Myocardial ischemia caused by reduced blood supply without any increase in myocardial oxygen demand may be temporary. A spasm of a coronary artery may restrict normal blood flow through it, and normal myocardial function returns once the spasm is relieved. More serious is a permanent injury to the myocardium, which may develop if ischemia persists for at least 15 to 20 minutes (according to present estimates). The ultimate variety of reduced blood and oxygen supply to the myocardium is permanent occlusion of a coronary artery by a thrombus, resulting in myocardial infarction.
Myocardial ischemia can have several effects on the heart—faulty contraction of the affected portion of the heart muscle (reduced or absent contractions); left ventricular failure, if the ischemia affects a large area of the myocardium; and, occasionally, ventricular arrhythmias. The consequences of temporary ischemia disappear either spontaneously or in response to interventions (such as taking nitro-glycerin), provided adequate blood supply is restored within the critical time limit.
Ischemia can be detected by means of the following diagnostic findings:
electrocardiographic changes consisting of a temporary shift of the S-T segment (fig. 27)
reversible abnormalities of isotopic perfusion scans performed in connection with stress tests (fig. 16, p. 39)
reversible abnormalities of left ventricular wall motion
Electrocardiographic abnormalities characteristic of ischemia may show up over the course of a Holter monitor test or during a treadmill exercise test. They may also appear when monitoring hospitalized patients during a spontaneous attack of chest pain.
In the treadmill stress test the workload on the heart is gradually increased by speeding up the treadmill and adding a slight incline. The goal of the test is to attain 90 percent of the predicted maximal heart rate during exercise for the person being tested (ranging between 120 and 150 beats a minute). A multilead electrocardiogram records during the test; the patient is also monitored for
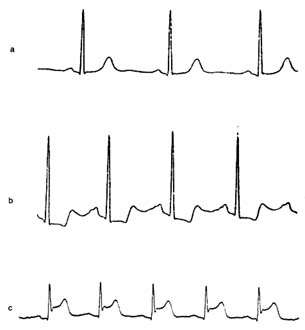
Figure 27. Single electrocardiographic leads exemplifying changes
produced by myocardial ischemia. (a) Normal configuration.
(b) Complexes showing depressed S-T segments, signifying moderate
myocardial ischemia (e.g. during treadmill exercise test), which return
to normal when the normal flow is restored. (c) Complexes showing
elevated S-T segments signifying severe ischemia (myocardial
injury), such as seen during early stages of myocardial infarction.
changes in blood pressure and the development of chest pain. In the presence of ischemia the S-T segment of the electrocardiogram shifts downward or, if ischemia is unusually severe, upward. Information concerning the severity of ischemia can be obtained from the extent of the S-T segment shifts, the amount of exercise required to provoke ischemia, and the time needed for the S-T segment to resume a normal position after the test. —
A Holter monitor test may reveal ischemia in the development of S-T segment depression during daily activities. Special equipment sensitive to S-T segment changes must be employed (the
primary objective of the Holter monitor test is the detection of arrhythmias). Spontaneous attacks of angina in hospitalized patients provide an additional opportunity to detect ischemia (or support its diagnosis) by observing temporary S-T segment shifts in the electrocardiogram during the attack of chest pain.
The diagnosis of ischemia by means of electrocardiographic abnormalities does have limitations. This method is most reliable when the control electrocardiogram (taken when the patient is at rest) is normal. Certain abnormalities in the control electrocardiogram may reduce the reliability of a test or even make a conclusive diagnosis of ischemia impossible.
The diagnostic use of isotopic scanning tests has been described in chapter 3. The test is performed in conjunction with the treadmill or pharmacological stress test and complements its findings. Whereas some indication of the severity of ischemia can be obtained from electrocardiographic changes, isotopic scanning can reveal the amount of heart muscle affected by the ischemia. Isotopic scan is of particular importance in cases where the electrocardiographic test is inconclusive or is incapable of supplying diagnostic information because of preexisting distortion of the complexes.
Under ordinary circumstances the electrocardiographic treadmill stress test is the principal means of diagnosing ischemia. Other procedures, such as the isotopic perfusion test and nuclide ventriculogram, steeply increase the cost of the diagnosis and are carried out only if specifically indicated.
Once ischemia has been diagnosed, further evaluation of the extent of coronary-artery disease is often made by means of coronary angiography (see chap. 3). The film taken after injecting the contrast material into the coronary arteries shows the distribution of blood through each coronary-artery system and displays any stenosis and occlusion of the branches (fig. 28). Angiography can also reveal collateral connections between arterial branches. This test is essential for determining the precise location of atherosclerotic plaques and evaluating the extent of coronary-artery disease. It is a prerequisite to such interventions as coronary angioplasty or bypass surgery. It should be emphasized, however, that tests for ischemia and angiography complement each other: angiography shows the lesion that may be responsible for ischemia but does not prove the presence of ischemia.
Figure 28. Coronary arteriograms (in actuality only one artery is visualized at a time).
(a) Normal coronary arteriogram. (b) Coronary arteriogram showing four areas of
severe stenosis (indicated by shaded circles). (Reprinted, by permission, from
Arthur Selzer, Principles and Practice of Clinical Cardiology
[Philadelphia: W. B. Saunders, 1983]).