Chapter Six
Arrhythmias
The healthy heart has a regular sequence of action. The process of impulse formation and its conduction from the pacemaker to the ventricles has been described in chapter 2. The regularity of the heartbeat, its rate, and the origin and spread of impulses all can deviate from the norm. The general term covering these abnormalities, regardless of their origin or significance, is arrhythmia , or disturbance of heart rhythm. The term is used even if the rhythm, or regular sequence of beats, is undisturbed but the rate is too slow or too fast.
The normal heartbeat is carefully regulated. At rest the rate is kept within relatively narrow limits, between 50 and 80 beats a minute in adults. During excitement and exercise the heart rate rises. The highest rate attained during strenuous exercise is between 160 and 200 beats a minute. The rhythm, under normal circumstances, is called sinoatrial rhythm (since it originates at the sinoatrial node) or sinus rhythm . It is customary to limit applying this term to moderate rates in the range of 50 to 100 beats a minute. When the heart rate exceeds 100 beats a minute, it is referred to as rapid rate, or tachycardia , regardless of whether it represents a normal phenomenon (such as during exercise) or an abnormal one. Conversely, a rate below 50 beats a minute is called slow rate, or bradycardia . Slow or rapid rate may originate in the normal pacemaker (sinus bradycardia and sinus tachycardia) or may be a manifestation of an abnormal rhythm. Abnormal ranges of impulse formation in the S-A node, when not caused by such factors as exercise, are usually related to signals from the autonomic nervous system and are
more often manifestations of disturbances outside the heart than of heart disease. For example, tachycardia can accompany fever or shock; bradycardia may be associated with fainting or nausea.
The normal rhythm of the heartbeat is almost perfectly regular. There are times, however, when an irregularity of the rhythm is entirely due to a normal variation of the firing sequence in the S-A node. Such irregularities are called sinus arrhythmias and are usually related to the breathing, such as slight slowing of the rate during inspiration of air and slight speeding during expiration. It is especially common in children.
It is important to recognize that these normal variants—sinus bradycardia, sinus tachycardia, and sinus arrhythmia—do not represent real disturbances of the heartbeat. Identification of their normal mechanism can be made with the aid of the electrocardiogram. They should not be confused with real disturbances of cardiac rhythm, which are customarily divided into abnormalities of impulse formation and abnormalities of impulse conduction.
The Mechanism of Arrhythmias
The heart contains other pacemakers than the S-A node, and they serve as emergency backup. These are the secondary pacemaker located in the A-V node and the tertiary pacemaker located in the cells of the Purkinje system (see chap. 2). Under certain conditions cells of other parts of the conducting system connecting the A-V node with both ventricles are able to initiate electrical stimulation of the heart; furthermore, most ordinary muscle cells, the role of which is contraction and relaxation, may under abnormal conditions take on the role of pacemaker. Ordinarily the secondary and tertiary pacemakers kick in only if an impulse from above fails to arrive; such single heartbeats or series of beats are said to be activated by default; they are referred to as escape beats , and a series of them represent an escape rhythm . However, these reserve pacemakers may assume an active role and discharge an electrical impulse out of turn, before the expected stimulation from above arrives. Such premature single impulses are called ectopic beats , and groups of them are called ectopic rhythms; they represent abnormal stimulation of the heart by usurpation (figs. 24–25).
Ectopic beats or rhythms may originate at any point of the conducting
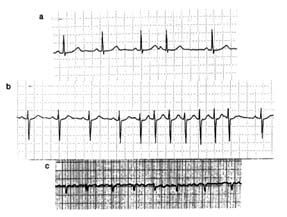
Figure 24. Atrial arrhythmias exemplified by strips of single electrocardiographic leads.
(a) Premature (ectopic) atrial beat (no. 4). (b) A short run (paroxysm) of atrial tachycardia
(seven beats). (c) Atrial fibrillation: there are no P waves, only rapid and irregular atrial
deflections; the response of the ventricular complexes is totally irregular.
system or even in abnormally stimulated heart muscle cells. Impulses originating in the upper part of the conducting system, including the A-V node, are termed supraventricular; their appearance in the electrocardiogram is identical with that of normal beats, as their impulses are transmitted along normal pathways to the ventricle, causing its depolarization and initiating its contraction. Ectopic impulses originating in the lower portion of the conducting system are called ventricular beats or rhythms. These impulses stimulate the ventricle in an abnormal sequence, which expresses itself in the electrocardiogram by wider, abnormal QRS complexes and T waves (fig. 25a).
Sequential ectopic beats are almost always at a faster than normal rate, that is, are ectopic tachycardias (supraventricular or ventricular). Supraventricular tachycardia can usually, though not always, be identified by electrocardiography as either atrial or junctional (A-V nodal) in origin. Occasionally it is associated with impulses traveling to the ventricle along abnormal pathways, shown in the electrocardiogram as wide complexes similar to those present in ventricular tachycardia.
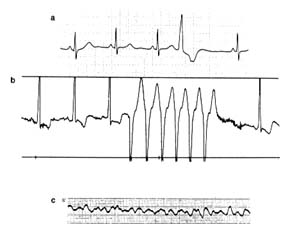
Figure 25. Ventricular arrhythmias exemplified by strips of single
electrocardiographic leads. (a) Premature ventricular beat. (b) A
short run (paroxysm) of ventricular tachycardia (seven beats).
(c) Ventricular fibrillation: chaotic, small, rapid complexes incapable of
maintaining coordinated heartbeat produce cardiac arrest. Note that
ventricular complexes in a and b are broader than, and
differ in shape from, normal complexes.
Abnormal activity of designated pacemaker cells or stimulated myocardial fibers is not the only mechanism for the origin of ectopic beats or ectopic rhythms. The alternative mode of production of arrhythmias is reentry , a phenomenon to which an important arrhythmogenic role has been attributed. To explain the concept of reentry, it is necessary to recapitulate some facts of normal electrophysiology. The cardiac conducting system transmits electrical impulses sequentially from the S-A node through the atrium to the A-V node, then along the bundle of His and its branches to the ventricles. This basically unidirectional conducting system is capable of conducting impulses in the reverse direction as well, though this does not take place under normal conditions. However, in the presence of arrhythmias impulses activating the ventricles may first send signals back to the atria, so that atrial contraction follows ventricular contraction. All cardiac cells (contractile myocardial cells as well as conducting fibers) have a refractory period: immediately
after a cell's designated function (contraction or conduction) is completed, there is a short time in which they do not respond to stimulation. The refractory period accounts for the fact that once the impulse reaches its final destination, it cannot travel backward. However, if there is an abnormal slowing within any portion of the conducting system (including its final pathway inside the ventricular muscle), the impulse may be reactivated when conduction is already responsive after the refractory period is over. The reactivated impulse may stimulate the ventricle into an additional (premature) contraction, an echo beat , and may travel forward or backward to any part of the heart, producing various arrhythmias.
An echo beat represents the simplest kind of reentry. More complex situations arise when the relationship between velocity of conduction forward and backward permits impulses to travel back and forth at regular, rapid rates (most frequently between 180 and 250 beats a minute), producing reentry tachycardia. Both supraventricular tachycardia (featuring narrow QRS complexes in the electrocardiogram) and ventricular tachycardia (featuring broad complexes) can be caused by reentry.
The electrocardiographic appearance of arrhythmias produced by abnormal impulse formation and that caused by reentry are almost identical and cannot always be differentiated. Yet such a differentiation can be of some practical importance because certain drugs may control one mechanism but not the other. Furthermore, certain varieties of reentry arrhythmias have been successfully treated by surgery.
More-advanced disturbances of the cardiac rhythm are flutter and fibrillation of the atria or the ventricles. The mechanism of these arrhythmias is somewhat similar to reentry: the electrical impulse is never extinguished but travels continuously through the affected portion of the heart. Atrial flutter produces a rapid, regular response, usually at a rate of 300 beats a minute, initiating a weak contraction of the atrial muscle. Because of their refractory period the ventricles are unable to respond to each atrial contraction, only to every other impulse (hence the ventricular rate is usually about 150 beats a minute, and the rhythm is regular). Atrial fibrillation occurs when the impulse travels through the atria at still-faster rates, leading to a chaotic twitching of the atrial muscle, which no longer can contract. The ventricles respond only to some
of the more powerful impulses and in an irregular fashion. The ventricular rate in atrial fibrillation (not influenced by drugs) is usually between 150 and 180 beats a minute, and its rhythm is totally irregular (fig. 24c). Flutter and fibrillation also affect the ventricles. But whereas the cardiac function can be maintained despite a weak or absent atrial contraction, ventricular fibrillation or flutter is tantamount to cessation of the circulatory function of the heart—cardiac arrest.
Disorders of Cardiac Conduction
The process of conduting impulses through the heart can be disturbed in three ways: (1) by a delay at a given point, (2) by its total interruption somewhere along the pathway, and (3) by nonresponsiveness of some part of the pathway.
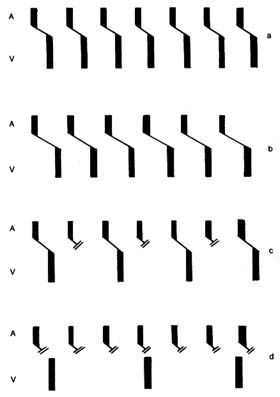
Abnormal delay in conduction usually occurs between the atria and the ventricles, presumably because something slows the transit of the impulses through the A-V node. Such a delay is shown in the electrocardiogram by the fact that the interval between the P wave and the QRS complex is prolonged beyond the normal 0.2 seconds. This phenomenon is called first-degree heart block or first-degree A-V block (fig. 26b). First-degree heart block does not disturb the rhythm or the rate of the heart. It is primarily detected by the electrocardiograph. Its importance lies in demonstrating that the patient's conducting system is imperfect, and it may precede more serious forms of conduction disturbances.
A higher degree of impairment of conduction between the atria and the ventricles is a second-degree heart (A-V ) block , a condition in which a certain number of impulses from the atria never reach the ventricle (figure 26c). Thus, one out of every two or more impulses from the atria is lost, producing dropped beats. The result may be an irregular heart action (if dropped beats occur every third beat or more) or a regular rhythm (if every other beat is dropped, two-to-one heart block ).
The next level of disturbance of atrioventricular conduction is its total interruption, third-degree heart (A-V ) block , also called complete heart (A-V ) block . Here the atria and the ventricles act entirely independently of each other: the atria contract as a result of the normal S-A mechanism; the ventricles contract as a result of a
Figure 26. Diagram showing the sequence of beats under normal conditions
and in various forms of heart block. The upper bar (A) represents atrial
depolarization, the lower bar (V) ventricular depolarization. The
oblique line joining the 2 bars is the atrioventricular conduction.
|
ventricular pacemaker with a slow rhythm unrelated to the atrial activity (fig. 26d). In complete heart block the atria usually maintain the normal heart rate of 70 beats a minute; the ventricles beat only 30 to 40 times a minute. This unusually slow ventricular rate imposes obvious problems on the maintenance of the circulation. In an otherwise sound heart the circulation can be maintained reasonably well, especially if the patient's activities are restricted; in the presence of serious heart disease such a low rate may precipitate heart failure. However, the principal danger of complete heart block lies in the fact that the ventricular pacemaker constitutes the last line of defense: its failure leaves the heart without any impulses, hence without contraction. Such failure of the ventricular pacemaker occasionally occurs in complete heart block for short periods (less than two minutes), causing loss of consciousness, and is known as cardiac syncope or Stokes-Adams attack . The danger of such an attack is self-evident: if it lasts more than four minutes, the patient will die.
The three degrees of heart block may be temporary or permanent. Temporary heart block may be due to acute, reversible illness, to the action of drugs, or to nervous influences; permanence implies complete, organic destruction of a given part of the conduction pathway.
If the interruption of conduction pathways occurs in the section below where the bundle of His divides into two branches, the impulse reaches the ventricle through the healthy bundle, so that the rhythm of the heart is not disturbed. However, if one of the ventricles fails to receive the impulses directly from the conduction pathways and the other ventricle is activated via a detour, the second ventricle contracts with a slight delay. This delay does not necessarily affect the function of the heart, but it causes gross distortion of the electrocardiogram. This type of conduction defect is called bundle-branch block (right or left, depending on which bundle is damaged). Bundle-branch block is a common disorder in some forms of heart disease, particularly in diseases of the coronary arteries.
Disturbances of the conduction system due to nonresponsiveness of the conducting tissues has already been touched on in connection with atrial flutter and fibrillation, in which not all rapid impulses can reach the ventricles. Other conditions in this category include atrioventricular dissociation , a disorder in which the A-V
node fires at an abnormally high speed, faster than the S-A node, and therefore takes priority in activating the ventricles. Nonresponsiveness of conducting pathways may separate these impulses from the atria, which obey the normal S-A node stimulation. This situation resembles complete heart block in that the atria and the ventricles beat independently of each other, although here, by contrast, the atrial rate is usually slower than the ventricular rate. Such conditions are almost always temporary, usually do not last long, and often reflect the influence of factors outside the heart (drugs or a disturbance of salt and water metabolism).
Significance and Consequences
of Arrhythmias
The function and efficiency of the cardiac pump under ordinary circumstances is not affected if the rhythm becomes irregular: the heart can adapt to an irregularity, even to the absence of effective atrial contraction. Arrhythmias frequently affect normal hearts in healthy individuals: monitor studies have shown that single ectopic beats can be found in almost one-half of the general population. Occasionally, healthy subjects display groups of ectopic beats (short runs of tachycardia), and even more complex arrhythmias sometimes appear. However, arrhythmias are more frequent in patients with heart disease and may produce serious consequences. The importance of arrhythmias in general is in its effect on cardiac function, its relationship to the underlying disease, and its role as a harbinger of life-threatening arrhythmias.
The function of the heart may be compromised if the heart rate is very fast or very slow. Tolerance of rapid tachycardia or slow bradycardia varies from person to person: in healthy populations only extremes in heart rate are likely to affect cardiac function; patients with cardiac disease, however, may be sensitive even to a moderate increase or decrease in heart rate, which may have serious consequences. The more common instances of arrhythmias in patients with organic heart disease, as already mentioned, may be an unimportant by-product of the underlying disease. But in some cases arrhythmias may accentuate the symptoms of the disease and affect cardiac function; in still others they may produce cardiac emergencies.
Perception of arrhythmias as palpitations is one of the symptoms that lead patients to seek medical care. As such, they may be a clue to the discovery of previously unknown, significant cardiac disease. Both healthy individuals having arrhythmias and patients with cardiac disease may be aware of the irregularity of their heartbeat. Even simple premature ectopic beats are often perceptible: ectopic ventricular beats usually cancel the next normal beat, producing a longer than usual pause that the affected person can feel as a skipping of heartbeats. Tachycardias often are perceived as palpitations or pounding of the heart. Yet some people, with or without heart disease, may be totally unaware of even the most complex arrhythmias.
Ventricular arrhythmias are potentially more serious than atrial arrhythmias, even though they are common in healthy persons. Since the most severe variety of ventricular arrhythmia is fibrillation—that is, cardiac arrest—some such arrhythmias need to be carefully studied to determine whether the patient is at a high risk of developing a fatal arrhythmia and thus requires aggressive treatment.
Common Arrhythmias
Paroxysmal atrial (supraventricular) tachycardia is characterized by sudden onset (perceived almost always as a pounding of the heart) and abrupt, spontaneous termination. It can last from minutes to several days. It often affects young, healthy persons: in some, attacks may recur only at long intervals; other may remain susceptible to frequent attacks, which can produce periodic disability. Many tachycardias respond to various maneuvers applied by a physician or even by patients themselves. These include applying pressure to the carotid artery in the neck, holding one's breath, or straining to force respiration, any of which may terminate an attack. Intravenous administration of certain drugs is more reliable in restoring normal heart rhythm. In rare instances, particularly when the rapid rate is poorly tolerated by the patient and unresponsive to drug therapy, it may be necessary to administer direct-current electric shock (cardioversion). As a general rule, no treatment of paroxysmal atrial tachycardia is needed between attacks; but if attacks recur frequently, preventive drugs can be prescribed.
Atrial flutter and atrial fibrillation are the most serious disruptions
of atrial rhythm. These two arrhythmias are related and may occur in the same patient. Both may develop in healthy persons but are more frequent in patients with various cardiac disorders. Atrial flutter and atrial fibrillation can be paroxysmal, that is, terminate within hours or days, or permanent, in which case normal rhythm usually should be restored by various interventions.
As mentioned, in atrial flutter the rhythm is regular and the heart rate (rate of ventricular contractions) is about 150 beats a minute since the ventricles respond to alternate atrial impulses. Drugs can partially block the pathways to every third impulse, reducing the rate to 100 beats a minute, or to every fourth impulse, lowering the rate to 75 beats a minute, thereby abolishing the tachycardia. Atrial flutter can in most cases be terminated by one of three methods: drugs, electric shock, or pacemaker stimulation of the right atrium (see chap. 4).
Atrial fibrillation is a much more common arrhythmia than atrial flutter; in fact, it is one of the most frequently encountered arrhythmias, particularly in patients over 60 years of age. Before the start of treatment the ventricular rate is usually within the range of 150 to 180 beats a minute, and the rhythm is irregular. Atrial fibrillation may develop as a complication of many cardiac disorders but most often results from mitral stenosis. The rapid rate of untreated atrial fibrillation, its major deleterious effect, is often poorly tolerated and may induce heart failure. Even in otherwise healthy persons atrial fibrillation may produce considerable discomfort, although it is unlikely to affect cardiac function. The rapid heart rate can be promptly and predictably reduced by drugs to a rate comparable to that of a normal, though irregular, rhythm, thereby alleviating the discomfort and other consequences. With a heart rate adequately controlled by a program of drug therapy, a patient may remain in atrial fibrillation for years and lead an active life. Thus atrial fibrillation is not a life-threatening arrhythmia. However, it does introduce a serious risk: the noncontracting atria can facilitate the development of blood clots attached to their walls, which can break loose and travel within the arterial system, producing emboli (clots occluding important vessels) and leading in some cases to stroke.
The approach to the treatment of atrial fibrillation involves two options: restoring normal rhythm or slowing the heart rate in patients remaining in atrial fibrillation. Normal rhythm can almost
always be restored either by drugs or by cardioversion. Restoration of normal rhythm is obviously the more advantageous option. But in patients prone to atrial fibrillation the arrhythmia may recur despite a course of preventive drugs. Patients who remain in atrial fibrillation are often given anticoagulants, drugs that inhibit clot formation, as protection against stroke. The choice of restoration of normal rhythm or control of the ventricular rate is usually made after estimating the probability of the arrhythmia recurring, which in turn may depend on the underlying cardiac disease.
Ventricular arrhythmias present one of the most difficult problems in cardiology. On the one hand, ventricular arrhythmias are ubiquitous in healthy adults; on the other hand, they can eventually result in fatal ventricular fibrillation. Consequently, a great deal of attention is given to recognizing and classifying them. Furthermore, ventricular arrhythmias are often closely linked to serious diseases of the myocardium, as evidence of electrical instability (the tendency to develop serious arrhythmias), and then require aggressive intervention.
Whereas the clinical importance of ventricular arrhythmias primarily depends on the underlying condition of the heart muscle, their appearance in the electrocardiogram often provides clues as to their prognostic significance. The simplest ventricular arrhythmia is the ventricular premature (ectopic) beat. However, its shape and timing in relation to the preceding normal beat may be telling. Ventricular ectopic beats that are alike and fixed in their timing are the least significant, except when they occur before the T wave of the preceding beat is completed. Ectopic beats varying in shape and timing may be evidence of electrical instability. Ectopic beats appearing in pairs or in groups of three are also considered potentially more serious. Ventricular ectopic beats appearing in runs of more than three beats are called ventricular tachycardia. All varieties of ventricular arrhythmia, including short runs of ventricular tachycardia, may be present in healthy persons; however, the more precarious the type of arrhythmia, the higher the probability of an underlying heart problem. Simpler ventricular arrhythmias do not affect heart function or cause discomfort.
Ventricular tachycardia plays a pivotal role in the evaluation of arrhythmias and in decisions regarding management, for under certain circumstances it can degenerate into fatal ventricular fibrillation.
Ventricular tachycardia is usually similar to supraventricular tachycardia in its effect on the circulation and in discomfort to the patient, but its prognostic implications are different. It is customary to classify ventricular tachycardia into two types, nonsustained and sustained . The former is characterized by spontaneous resumption of normal rhythm; the latter persists until terminated by intervention. Nonsustained tachycardia may not compromise health; sustained tachycardia is always considered serious. Ventricular flutter and ventricular fibrillation are the commonest causes of cardiac arrest. As a rule, ventricular fibrillation is fatal unless treated immediately. Occasionally, however, ventricular flutter and fibrillation appear in nonsustained form, and normal rhythm spontaneously resumes in less than four minutes, in which case they result in cardiac syncope (see chap. 7).
Evaluation of ventricular arrhythmias requires two steps: recognition of the type and frequency of arrhythmia and diagnosis of its cause, including any underlying heart disease. An ordinary electrocardiogram is inadequate for diagnosing the extent of the arrhythmia. For that purpose it is necessary to record a continuous electrocardiographic tracing by means of a Holter monitor, which can display every heartbeat over a 24-hour period. An alternate method is continuous electrocardiographic monitoring of patients in an appropriate unit in a hospital; important arrhythmias observed on the video display are then printed out for further examination.
In evaluating the background of the arrhythmia, the physician considers the state of the heart, especially the presence of heart disease, and the possible specific causes of arrhythmias, such as acute myocardial infarction, myocardial ischemia, the toxic effect of a drug, abnormalities of electrolytes or acid-base balance, and certain abnormalities of renal or hepatic function. If the ventricular arrhythmia is of a serious variety and none of the reversible causes can be identified, except for the presence of myocardial disease, further tests may be indicated, including an electrophysiological study. Here the patient is taken into a cardiac catheterization laboratory, where a pacing wire is introduced into a cardiac ventricle. The heart can then be stimulated through the wire by an electronic pacemaker outside the body to determine whether an appropriate stimulus can initiate a nonsustained or sustained ventricular tachycardia. Such pacing studies can also be used for testing responses to
antiarrhythmic drugs. In patients in whom the pacing stimulus induces a ventricular tachycardia, stimulation is repeated after a drug is administered: if tachycardia can no longer be induced, the drug may be considered efficacious in preventing naturally occurring attacks. However, there is still some controversy as to whether suppression of artificially induced tachycardia translates into reliable prevention of future attacks.
Treatment of ventricular arrhythmias includes both prophylactic and remedial therapy. The latter is rather limited, involving emergency treatment of ventricular tachycardia and ventricular fibrillation, termination of tachycardias, and the elimination of frequent premature beats that may produce discomfort or disability. Prophylactic therapy is the principal goal of antiarrhythmic treatment and includes a wide range of approaches. The most important caution in initiating prophylactic therapy of ventricular arrhythmia is that antiarrhythmic drugs carry a definite risk to the patient. Some have undesirable side effects that may unfavorably affect quality of life; furthermore, drugs may compromise the function of vital organs such as the blood, liver, and kidneys. And in about 10 percent of patients arrhythmias could be made worse by such drugs, owing to a paradoxical action. Thus the physician has to balance the risk of antiarrhythmic therapy against the risk of serious arrhythmias developing in the future. Short-range antiarrhythmic therapy, such as may be indicated in acute myocardial infarction, presents no problem; but the persistence of ominous arrhythmias may require lifelong antiarrhythmic therapy, which—particularly in patients who have no symptoms—poses a serious dilemma as to whether and when treatment is indicated. In the minority of cases successful treatment may be accomplished if a clear cause of ventricular arrhythmias can be identified and eliminated.
In general, certain priorities are assigned in initiating antiarrhythmic therapy. The first priority is given to patients who have been resuscitated from cardiac arrest. Second, aggressive therapy is usually needed for patients with recurrent sustained ventricular tachycardia. Last, patients with less-serious ventricular arrhythmias are often grouped according to the precariousness of the observed arrhythmias and the severity of underlying heart disease. Those with no evidence of organic heart disease usually require no treatment; those with myocardial disease are treated aggressively,
particularly if myocardial function is seriously impaired. During the 1980s a large number of new antiarrhythmic drugs were introduced and approved by the Food and Drug Administration, and others are still being tested. So far no drug has been produced that is highly effective yet devoid of undesirable effects.
In patients with demonstrated life-threatening arrhythmias, more-drastic interventions are available, such as surgery. The principle behind a surgical approach to the treatment of ventricular arrhythmias is the hypothesis that most serious arrhythmias involve the reentry phenomenon: if the pathway of reentry could be identified and interrupted, further arrhythmias could be prevented. Surgical incision of areas of the endocardium (the inner layer of the heart) determined by electrophysiological studies as likely reentry pathways has eliminated serious arrhythmias in some cases. However, such operations (requiring open-heart surgery) have not been uniformly successful. The possibility that similar results could be obtained by the simpler method of introducing a cardiac catheter into the heart and producing damage (either by burning or freezing) to a critical area of abnormal conduction is now being tested.
Patients who have been resuscitated from cardiac arrest caused by documented ventricular fibrillation can now be treated by automatic defibrillators, which can recognize ventricular fibrillation and immediately apply an electric shock capable of terminating the arrhythmia. This treatment requires surgical introduction of a wire into the surface of the heart. Initial experience with automatic defibrillators has been satisfactory, though they have not proven to be without risk.
Other Arrhythmias
Heart Block and Other Bradycardias
The interruption of conducting paths connecting the atria with the ventricles produces heart block. Impulses from the atria cannot reach and activate the ventricles, which then are at the mercy of a rather weak tertiary pacemaker, located within the ventricles, which becomes responsible for the contraction of the ventricles and thus the pumping function of the heart. The rhythm of the ventricular pacemaker is slow, averaging 30 beats a minute, and it is undependable because of occasional periods of further slowing or even
interruption of its action altogether (ventricular standstill ). Bradycardia of 30 beats a minute may be tolerated by a patient, though it limits activity. Bradycardia at a rate less than 20 beats a minute may produce temporary loss of consciousness, as does ventricular standstill. Complete heart block and its complications are the principal target of electronic pacemaker therapy.
Disturbance of the upper division of the conducting system, that located within the atria, and malfunction of the primary pacemaker may also produce excessive slowing or stoppage of the electrical impulses activating cardiac action. If such malfunction is not compensated for by emergency action of the lower pacemakers, the patient may experience such symptoms as dizziness or even loss of consciousness (sick-sinus syndrome). The fundamental difference between malfunction of the upper and lower divisions of the conducting system is that the former slows or stops the total action of the heart—both the atria and the ventricles—whereas the latter does not affect the atria, which may function normally (and may speed up normally with exercise); the ventricles, however, respond to a slow and fixed rate initiated by the ventricular pacemaker, which is unrelated to the rhythm of the atria.
Both varieties of the malfunction of the conducting system, manifested as excessively slow heart rate or as pauses, may occur under certain circumstances in healthy persons. Pronounced sinus bradycardia (rates as low as the high thirties) may be present as a result of athletic training and be a desirable adaptation. Excessive sinus bradycardia or pauses may also represent a response to certain reflexes, such as those initiated by nausea or cough, in which case the person may experience faintness or syncope. Drugs that slow the heartbeat may produce symptomatic serious bradycardia. In the absence of heart disease these types of temporary complete A-V block do not usually develop, with one exception: some persons are born with an abnormal conducting system (congenital complete heart block), which may be associated with other congenital defects or may appear as the sole abnormality. They frequently exhibit much faster ventricular rates than those who suffer from acquired heart block and can lead an active life, often unaware of this problem.
Complete heart block (lower-division malfunction), more often than not, is permanent. But it may also develop as a temporary phenomenon in the course of acute disorders, such as acute myocardial
infarction, or following cardiac operations, or in response to certain stimuli in patients who have lesser conduction disturbances (first- or second-degree heart block). Assessment of potential danger from temporary bradycardia or pauses due to complete heart block can usually determine whether treatment is necessary or one can safely wait for the return of normal rhythm. One of the criteria in this decision is the rate and stability of the emergency substitute pacemaker.
As mentioned, the electronic pacemaker is the principal therapeutic tool in severe bradycardias, playing either a remedial or a prophylactic role. The remedial use of the pacemaker is needed in the great majority of cases of permanent, complete heart block as well as occasionally in permanent, severe sinus bradycardia. In most other bradycardias pacemakers are implanted as a standby. Serious conduction disturbances developing in the course of acute cardiac diseases often require the temporary use of a pacemaker, in which case the pulse generator is placed outside the body.
Permanent pacemaker therapy involves two decisions—whether a pacemaker is needed and, if so, whether a single-chamber or dual-chamber unit is indicated. The single-chamber pacemaker can operate in a remedial or standby role, stimulating the atria or the ventricles; it is the less expensive of the two, simpler in design and probably longer-lasting. Dual-chamber pacemakers can sense abnormal slowing of atria or ventricles and stimulate the appropriate chamber; furthermore, they can transmit normal sinus impulses from an atrium to a blocked ventricle, preserving the normal interval between them. The most important use of the dual-chamber pacemaker is in patients with permanent complete heart block, whose atria usually respond to the normal sinus node impulses but whose ventricles beat at an independent, slow, fixed rate. Here the normal variation of the heart rate in response to exercise or excitement displayed by the atria can be transmitted to the ventricles, which with a single-chamber pacemaker would operate at a fixed rate.
Preexcitation Arrhythmias
The phenomenon of preexcitation , known as Wolff-Parkinson-White syndrome , is related to a congenital abnormality of the heart in which an accessory tract conducts impulses from the atria to the
ventricles. This tract is located in a different part of the heart than the normal conduction system. It can short-circuit the conduction between the two chambers (the normal impulse is delayed within the A-V node) and stimulate prematurely certain portions of the ventricular muscle. As a result, the electrocardiogram shows a pronounced distortion of the QRS complexes, which could be mistaken for serious heart disease. Yet in most persons with this abnormality the heart is structurally and functionally normal in all other respects, and they remain unaware of the existence of this anomaly until they undergo an electrocardiogram for some unrelated reason. In a small number of such persons, however, the abnormal bypass tract is a source of disabling or even life-threatening arrhythmias. The disparity between the conduction time through the normal channels and the bypass tract may under certain circumstances cause reentry tachycardias, which permit an impulse reaching the ventricle by way of either tract to return to the atrium via the other pathway. If atrial fibrillation or flutter develops, there may be an unusually rapid ventricular rate—up to 300 beats a minute—which normally would be averted by the A-V node. Some patients can be treated medically by antiarrhythmic drugs. If no effective and safe drugs for controlling the arrhythmias can be found, catheter ablation can be performed to sever the abnormal tracts. This procedure has been found more consistently successful than other catheter ablation used in controlling intractable tachycardias. If catheter ablation fails, a surgical ablation may be used.