Interventional Cardiac Therapy
Traditionally treatment of heart disease fit into two classes, medical and surgical. Now a third mode of treatment is available and widely
used, intermediate between medical and surgical—interventional therapy , performed by specially trained cardiologists rather than cardiovascular surgeons. Some of these procedures represent alternatives to surgery; in selected cases they may be equally effective yet simpler and less expensive and require the patient to spend much less time in recovery. Others have specific uses and indications. Among such procedures are
balloon coronary angioplasty (percutaneous transluminal coronary angioplasty, or PTCA)
balloon valvuloplasty
temporary or permanent use of pacemakers
intraaortic balloon pump
interventional treatment of arrhythmias
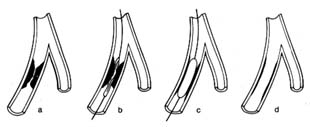
Coronary angioplasty was developed in the late 1970s, and it has proven successful in relieving stenosis of the larger branches of the coronary arteries. Atherosclerosis of arteries produces plaques that reduce the amount of blood the artery is able to deliver to the affected organ. When such plaques significantly reduce the lumen of a coronary artery and are accessible, as demonstrated by coronary arteriography, angioplasty is performed by introducing a specially designed cardiac catheter into the arterial system. At one end of the catheter is a balloon, which when deflated fits snugly around the catheter; a separate channel connects it with the end of the catheter outside the body, through which it can be inflated. The inflated balloon has a long, cylindrical shape of fixed diameter, which can widen the tip of the catheter considerably, filling the inside of the artery. Under fluoroscopic examination the tip of the catheter is placed in the portion of the coronary artery narrowed by the plaque. The balloon is then inflated with a liquid at controlled and measurable pressure, compressing the plaque and thereby greatly reducing the stenosis (fig. 19). Cutting devices, lasers, and small framework-like devices called stents can be used in difficult cases.
The success of coronary angioplasty in improving blood supply to the heart by relieving obstruction in a coronary artery encouraged the development of a similar technique to relieve valvular narrowing. Balloon valvuloplasty works on the same principle as PTCA;
Figure 19. Coronary angioplasty. (a) Coronary branch showing severe stenosis.
(b) Catheter placed in this branch with a deflated balloon at the level of the stenosis.
(c) Inflated balloon compressing the stenosing plaques.
(d) Minimal residual stenosis after the removal of the catheter.
the catheters and balloons are appropriately larger, and they differ in design. The catheter tip with deflated balloon is placed at the stenosed valve, which widens when the balloon is inflated.
Electronic pacemakers have been in use since the 1960s. They were introduced to provide protection from sudden death caused by failure of the natural pacemaker. The artificial pacemaker consists of a generator that rhythmically discharges electrical impulses. It is connected with an insulated wire inserted through the patient's venous system, so that its exposed tip is in contact with the muscle of the right ventricle or right atrium or both. The pacemaker has two functions: pacing , i.e. generating rhythmic electrical impulses, and sensing , i.e. detecting electrical impulses from the beating heart, which inhibit the artificial impulses from the generator. The sensing function permits the pacemaker to become active only when needed, assuming a standby function in patients who develop temporarily excessive slowing of the heart, or "pauses" (chap. 6). In patients with permanently slow heart rhythm the electronic pacemaker operates at all times. The point of stimulation of the heart is selected in accordance with the type of bradycardia (abnormally slow heartbeat): in diseases of the sinus node the atrium is stimulated; in complete heart block, the ventricle.
The pacemaker can be set up as a temporary measure, with the stimulating wire inside a cardiac chamber connected to a generator located outside the body. More often, however, pacing is permanent, in which case a miniaturized generator is placed under the skin in a small pocket made by surgical incision, usually underneath the collarbone. In permanent pacemakers the generator
imbedded under the skin can be programmed from outside the body to adjust the heart rate.
Pacing has now become quite sophisticated. The most important development has been the dual-chamber pacemaker . Separate wires are introduced into the atrium and the ventricle. The generator can sense and initiate pacing of the atrium, if that chamber fails to receive the normal stimulus, or the ventricle, if the atrial impulse fails to reach the ventricle. Furthermore, if needed, both chambers can be sequentially paced, maintaining the natural interval between them.
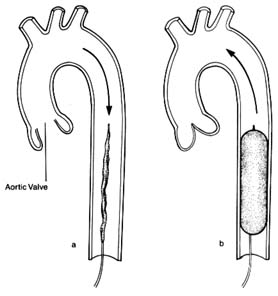
Intraaortic balloon pumps act as boosters supporting the pumping action of a failing left ventricle. Inasmuch as such devices can safely be used for no more than a few days, this method of treatment is intended only to tide over a temporary malfunction of the left ventricle. A specially designed catheter is introduced into an artery in the groin and advanced into the descending aorta. The catheter is surrounded by an inflatable balloon along most of its length. The deflated balloon is connected to a pump (outside the body), which is synchronized with the heart action by means of signals coming from an electrocardiogram. During cardiac systole the balloon remains deflated; during diastole, when the aortic valves are closed, the pump inflates the balloon, which fills the inside of the aorta, thereby acting as a pump and displacing the blood (fig. 20). By this means the blood flow into the critical areas—the brain and the coronary circulation—receives an additional boost in diastole, supplementing the normal pumping action of the heart in systole; furthermore, this technique helps maintain blood pressure at an adequate level. The principal use of the intraaortic balloon pump is in the treatment of shock, particularly when it is caused by failure of a cardiac ventricle; it is also used in treating unstable angina pectoris (chap. 7) and in stabilizing some patients after open-heart surgery.
Interventional treatment of arrhythmias includes the following techniques:
external defibrillation of the heart in cardiac arrest
termination of tachycardias by electric shock (cardioversion) or by means of pacemakers
deliberate induction of damage to the conducting system of the heart by means of special catheters to control certain life-threatening arrhythmias
Ventricular fibrillation , uncoordinated twitching of the heart muscle, is the commonest cause of cardiac arrest. The heart ceases to pump blood, effectively, and the condition is fatal unless it can be reversed within four to five minutes. External defibrillation , application of electric current to the outside of the chest in the region of the heart by means of two conductive paddles, may restore normal heartbeat—the essential step in cardiac resuscitation.
Figure 20. Intraaortic balloon pump. A deflated balloon is placed in the descending
aorta and is connected with a pump, the action of which is synchronized with
cardiac contraction and relaxation by means of an electrocardiographic signal.
(a) During ventricular systole (open aortic valve) the balloon remains deflated
and blood flow is normal. (b) During ventricular diastole (closed aortic valve)
the balloon is inflated and displaces the blood in the descending aorta.
A related technique is used to restore a normal heart rhythm in certain arrhythmias involving tachycardia , abnormally rapid heart action. Here, however, the electric shock has to be delivered at a specific point in the cardiac cycle and must be synchronized by an electrocardiographic signal. This procedure, cardioversion , may be applied in emergencies for acute arrhythmias or electively for chronic arrhythmias. Whereas in cardiac arrest defibrillation is performed on unconscious patients, candidates for cardioversion, a very painful procedure, are conscious and hence have to be put under general anesthesia or heavy sedation.
A new application of the technique of treating arrhythmias electrically is the implantable defibrillator and cardioverter , which has been approved for limited use. At present this apparatus has to be inserted surgically, its wires sutured to the surface of the heart and its generator implanted under the skin. The objective of this method is to defibrillate automatically patients who develop ventricular fibrillation or to cardiovert ventricular tachycardia, thus preventing cardiac arrest. The generator is programmed to sense and diagnose ventricular fibrillation or ventricular tachycardia and to administer an appropriate electric shock to restore regular rhythm. The treatment is indicated only in patients with a clearly demonstrated high risk of fatal arrhythmia.
Certain tachycardias can be terminated by delivering rapid impulses by means of an electronic pacemaker placed temporarily with its tip in the right atrium. This method, pacing overdrive , is an alternative to cardioversion; it has the advantage of being painless, thus obviating the need for anesthesia.
A new method of treatment of certain serious arrhythmias originating in the atrium is now being developed and tested. Certain atrial arrhythmias occurring periodically may cause serious disability and be unresponsive to drug therapy. It is possible, by manipulating a specially designed catheter, to destroy the tract conducting impulses from the atria to the ventricles (the atrioventricular node or bundle of His), thereby shielding the ventricles from the rapid stimulation. Certain abnormal pathways can be destroyed while preserving the normal pathways. In some cases permanent pacemakers may be necessary after such an ablation procedure. Obviously, such a drastic step should be taken only if other means of controlling the heart fail.