Chapter Three
Diagnosis
Case Finding
The discovery of a previously unknown health problem, or case finding, may occur when an abnormality is found during the routine medical examination of a healthy patient or when a person becomes aware of a change in his or her state of health and seeks medical care. Periodic health examinations and examinations requested by someone's employer or insurer vary greatly in scope and thoroughness. A physical examination is mandatory. A variety of tests may be included in the examination, such as blood tests, an electrocardiogram, a chest X-ray, and treadmill stress tests. Some findings raise suspicion that a heart problem may be present:
abnormal heart sounds or murmurs
irregularities of the rhythm of the heart
elevated blood pressure
unusual shape or enlargement of the heart shadow in the X-ray film
abnormalities shown in the standard electrocardiogram
electrocardiographic abnormalities detected during a treadmill stress test
The discovery of an abnormality in a routine examination usually results in further evaluation to confirm or reject the suspicion of heart disease. Occasionally, findings are characteristic enough to make a firm diagnosis at once. Heart disease present at birth—congenital heart disease—may be discovered in the postnatal examination
or in a periodic examination performed during the first year of life.
The discovery of a previously unknown heart abnormality is a goal of preventive cardiology, but the commonest way heart disease is first detected is when a person becomes aware of certain symptoms and seeks medical care. Symptoms may signal an acute change in the state of health, requiring immediate attention, or they may be nondisabling and repetitive.
Acute events that may demand emergency medical care include sudden loss of consciousness, severe dizziness or faintness, severe chest pain, severe shortness of breath, or sudden onset of rapid heart action. Chronic or repetitive symptoms that most frequently lead to the discovery of heart disease are shortness of breath, chest pain, and palpitations.
Shortness of breath is a normal response to strenuous exercise and as such is not alarming. However, shortness of breath provoked by minor, previously well-tolerated activity or occurring during rest makes a patient aware of an abnormal respiratory effort. This abnormal shortness of breath, most often associated with diseases of the heart or lungs, is called dyspnea . Dyspnea may appear in patients resting in bed as a sudden onset of rapid breathing, often accompanied by coughing, or as discomfort when lying down if the patient can breathe comfortably only when sitting up. A special variety of dyspnea, hyperventilation, in which a person is compelled to breathe deeply and rapidly, is usually unrelated to serious abnormalities of the heart, being a response to abnormal signals from the brain that may occur in some anxious, otherwise healthy persons. As a manifestation of heart disease, dyspnea is usually related to impaired function of the left ventricle (see chap. 5).
Chest pain is the principal symptom of coronary disease. Inasmuch as chest pain may be produced by a variety of conditions, some inconsequential, identification of the cause of chest pain constitutes a real challenge to the physician. Other causes of chest pain include pericarditis, aortic dissection, spasm of the esophagus, and pleurisy. In many cases, chest pain originates in the muscles or nerves within the chest wall and does not indicate a significant health problem.
Ordinarily a person is not aware of the beating of the heart, although it often seems to "pound" during strenuous exercise, excitement,
or fright. Palpitations refer to unprovoked perception of unusual heart action, often occurring at rest. A patient may recognize the heart beating too slowly, too fast, or irregularly. Thus palpitations suggest an abnormality of the rhythm of the heart (arrhythmia ).
These three symptoms motivating a person to seek medical care account for the majority of discoveries of a previously unknown heart disease. They may, however, indicate a health problem of a different nature, or none at all. Less frequently, heart disease is discovered in patients who consult physicians for other symptoms: dizziness, excessive weakness, fainting attacks, swelling of ankles, abdominal discomfort, and so on.
The Initial Medical Examination
In the initial contact with a patient suspected of having heart disease, the physician takes a complete medical history and performs a physical examination. The medical history is largely devoted to a detailed analysis of the patient's symptoms. The patient's ability to present a well-observed, reliable, and consistent account of symptoms is essential in helping the physician draw correct conclusions. The medical history also includes background information, such as past medical problems, a family medical history, a social and occupational assessment, and an evaluation of the patient's personality.
During the initial interview the physician takes note of the patient's general appearance and his or her concern regarding the possibility of serious illness. Certain abnormalities may become obvious: shortness of breath while talking, unusual pallor, cyanosis, and strain in performing minor activities such as walking into the room or dressing. Such observations do not necessarily point to a heart problem but could, supported by the patient's history, make the physician suspect heart disease.
A complete physical examination focuses on those areas of concern revealed in the history taking and initial observations. The contribution of the physical examination to the diagnosis of heart disease varies widely: sometimes, although serious heart disease is present, the findings of the physical examination may be normal; at other times, a definitive diagnosis can be made on the basis of the medical history and physical examination without further tests.
Cardiac auscultation—listening to the heart with a stethoscope on the front of the chest—is an important part of the examination. In a healthy person cardiac auscultation reveals two normal heart sounds produced by the action of heart valves. Abnormal findings suggesting heart disease include certain alterations of the normal sounds and the presence of additional sounds and heart murmurs. Heart murmurs occur when a normal, smooth, "laminar" blood flow becomes turbulent. Turbulence arises when there is an obstacle in the path of blood flow, such as narrowing of a heart valve, backflow through an incompetent heart valve, or an abnormal communication between the right and the left sides of the heart or between certain large blood vessels. (Murmur due to turbulent flow may be present in healthy subjects as well, particularly in children after acceleration or increase of blood flow such as during exercise. Such murmurs are usually referred to as "functional" or "innocent.") Thus the discovery of a heart murmur can help the physician diagnose diseases of heart valves and certain congenital defects of the heart. Other abnormal findings on auscultation include a "friction rub," usually indicating pericarditis; extra heart sounds, which may be related to impaired function of the heart; and abnormal clicks or snaps originating in malfunctioning valves.
Other parts of the physical examination providing diagnostic information in heart disease include taking the arterial pulse, observing the venous pulse, and measuring the blood pressure. Serious malfunction of the heart (congestive heart failure ) may be signaled by abnormalities of the venous pulse in the neck, the presence of rales (bubbling noises during breathing), enlargement of the liver, and the accumulation of fluid in the ankles, around the lungs, and in the abdominal cavity. A physician can perceive abnormalities of the heart rhythm by feeling the pulse at the wrist. However, a more detailed analysis requires listening to the sequence of heartbeats with the stethoscope, sometimes combined with observing the venous pulse.
After completing the medical history and physical examination, the physician can sometimes establish a definitive diagnosis or rule out heart disease. Usually, however, the result of the initial workup is a tentative diagnosis or a list of illnesses to be considered. The next step is to select further diagnostic procedures. A wide range of tests is now available to aid in the diagnosis of heart disease, from
simple ones performed in the office to complex hospital procedures, some entailing risk to the patient. It is customary to classify diagnostic heart tests as noninvasive , wherein all instruments used in the test remain outside the body, and invasive , requiring the introduction of catheters or other instruments into the body. Invasive diagnostic procedures also include certain minor operations.
Noninvasive Tests
Electrocardiography is one of the two oldest, most widely used, and least expensive tests in the diagnosis of heart disease. The electrocardiogram , developed for practical use at the turn of the century, records the electrical potential generated by each heartbeat. The contraction and relaxation of the heart muscle is caused by a flow of electrolytes (sodium, potassium, and calcium) in and out of each muscle cell through the surrounding membrane. This flow generates a week electrical current. Each muscle cell of the heart is a miniature battery discharging electricity with each contraction (depolarizing), and recharging itself during relaxation (repolarizing). The electrocardiograph is an amplifier capable of picking up this weak current from the surface of the body. The electrical potential generated over time by the millions of heart muscle cells—between 0.1 and 2.0 millivolts, or about one millionth the voltage of household current—displayed continuously on a roll of graph paper, is the standard electrocardiogram. It consists of 12 leads recorded with electrodes placed on various points on the chest, both arms, and the left leg, thus providing electrical "views" of the heart from various angles.
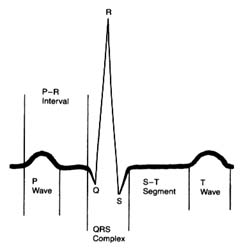
An electrocardiographic image produced by a single heartbeat is shown in figure 12. Any deviation from the horizontal line, or baseline , whether above (positive potential ) or below (negative potential ), denotes electrical activity. Each change of potential is called a wave . The first is a positive, broad, triangular wave called the P wave , representing depolarization of the two atria and signaling their contraction. It is followed by a return to the baseline, called the P-R interval . Next comes a complex consisting of three sharp waves: a small, negative Q wave , a tall, positive R wave , and a small, negative S wave . These three waves together constitute the QRS complex , which shows depolarization of the two ventricles
Figure 12. A typical electrocardiographic lead showing the various
components of the electrocardiogram.
coinciding with the onset of ventricular contraction. A flat, electrically inert baseline follows (the S-T segment ), after which the slower and lower T wave appears, indicating repolarization of the two ventricles. The section of the electrocardiogram including the QRS complex, the S-T segment, and the T wave is referred to as the ventricular complex . The end of the T wave is referred to as the ventricular complex . The end of the ventricular contraction occurs during the descending part of the T wave. Absence of electrical activity is displayed by the horizontal baseline between the end of the T wave and the beginning of the P wave of the next beat, during which time the ventricles relax.
The normal electrocardiogram shows a sequence of evenly spaced complexes. Experience has established the limits of normal variation in the height and direction of the five waves in healthy persons according to age group. The abnormal electrocardiogram may indicate two types of deviation from these norms: abnormalities of the sequence of beat (arrhythmias) and abnormalities of the waves and the baseline segments between them (abnormalities of electrocardiographic contour). The normal heart beats evenly at a rate ranging between 60 and 150 beats a minute. Irregular spacing of heartbeats demonstrates an arrhythmia, a disturbance of the rhythm of the heart. The electrocardiogram is the principal tool for
diagnosing cardiac arrhythmias, since it shows the rate and regularity of heartbeats; the shape, direction, and relationship of the P waves to the other complexes, including the absence of P waves; and deviations in the contour of the QRS complexes and T waves in the abnormally spaced beats.
The electrocardiogram is an indispensable tool in recognizing and analyzing arrhythmias. An equally important role of the electrocardiogram is to provide information concerning the state of the heart muscle on the basis of certain alterations in the electrocardiographic complexes, especially the QRS-T part. This feature of the electrocardiogram, however, requires more cautious interpretation because alterations produced by changes in the heart muscle are less specific than those produced by arrhythmias. Alterations in the electrocardiogram helpful to the physician may result from myocardial infarction and from enlargement of one or both cardiac ventricles or atria. These changes tend to be a permanent feature of a given person's electrocardiogram. In addition, daily and hourly variations may suggest acute changes in the state of the heart muscle, such as ischemia, acute pericarditis, and imbalance of electrolytes. In some healthy persons electrocardiograms may deviate from the norm without indicating any heart problem; these are referred to as normal variants. By contrast, many electrocardiographic abnormalities—perhaps the majority—are inconclusive, or "nonspecific." Here the significance of the changes has to be evaluated by means other than the electrocardiogram.
Electrocardiography is the most universally and frequently used aid in the diagnosis of heart disease. Yet it has its limitations: a normal electrocardiogram can be present in patients with a serious heart problem, and an abnormal electrocardiogram does not automatically indicate significant heart disease.
Electrocardiographic techniques are also incorporated in certain other cardiac tests. The treadmill stress test helps evaluate the effect of increased work on the heart by monitoring it electrocardiographically while the patient exercises on a treadmill. The principal indication for this test is a suspicion of coronary-artery disease, which may reduce the oxygen supply to some part of the heart muscle (ischemia) during exercise. Occasionally exercise may provoke arrhythmias (see chap. 8), and this test is used to detect them. The Holter monitor test is a 24-hour survey of heart rhythm. The
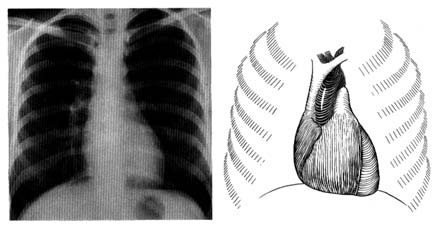
Figure 13. A radiograph (X-ray) of the chest in the anteroposterior view in a healthy person (left).
A reference diagram (right) shows the heart and the great vessels in relation to the rib cage.
Compare with figure 2 to identify cardiovascular structures.
patient wears a specialized tape recorder that registers every heartbeat. A computer analysis of the recording reveals any disturbances of heart rhythm. Newer, high-fidelity recording equipment may pick up indications of ischemia of the heart muscle. The electrocardiogram is an important aid in diagnosing some acute diseases of the heart or monitoring the heart during surgical procedures (cardiac or noncardiac). In such cases the heart rhythm is sensed by one or two electrocardiographic leads and is displayed continuously on an oscilloscope. This procedure is standard in intensive-care wards, including coronary-care units.
Radiography is the second traditional diagnostic aid in heart diseases. Because X rays penetrate certain tissues better than others, X-ray photography permits considerable differentiation of body structures. The chest X ray displays three types of shadows: the heavy shadow of bony structures (spine, ribs), the light shadow of lungs filled with air, and the intermediate shadow of the heart and blood vessels (fig. 13).
Radiographic examination can display enlargement of the heart and the great vessels arising from it as well as the distribution of blood vessels throughout the lungs. Newer technology (especially echocardiography) provides a more accurate method of recognizing
enlargement of the individual heart chambers or other structures in the X-ray shadow of the heart. Today cardiac radiography is used more as a screening technique and a means of assessing changes occurring between examinations than as a way of definitively diagnosing cardiac enlargement. This test, however, is indispensable in displaying fluid in the lungs, an important feature of heart failure. (Current technology has produced some specialized radiological techniques in diagnosing heart disease. These will be discussed later in the chapter in connection with invasive tests.)
Blood tests usually play an important role in diagnosing diseases, but not in the case of heart ailments. Only three sets of blood tests are a regular part of diagnostic work in cardiology: measurement of cardiac enzymes in acute myocardial infarction; measurement of cardiac drug levels in the blood to regulate dosage; and blood culture for discovery of bacteria if infection of the heart is suspected.
Echocardiography has revolutionized the diagnosis of heart disease since it was first applied in the 1960s. Like other ultrasound techniques, it produces an image by transmitting high-frequency sound waves (ultrasound), which reflect off different structures of the body with varying intensity; the resulting data show the interface of those structures.
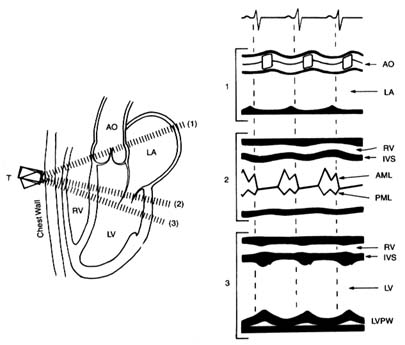
In the original echocardiographic technique, an electronic wand—a transducer—is pressed against the patient's chest and pointed in the direction of the heart, toward which it sends ultrasonic waves. The heart muscle, its neighboring structures, and cavities filled with blood vary in density, and the transducer picks up those variations in the reflected sound, which it converts into an electronic signal that is recorded on moving paper. The echocardiographic record shows not only changes in the size of the cardiac chambers during ventricular contraction and relaxation but also the rapidity of contraction and relaxation—points of some importance in evaluating heart function. This method, M-mode echocardiography , displays a one-dimensional view of the portion of the heart at which the transducer is aimed. It is often referred to as the "icepick" view of the heart because the narrow sound beam drives straight through the heart like an icepick through a solid block (fig. 14). M-mode echocardiographic display provides some information that previously required invasive tests, such as the size (width) of each heart chamber, the thickness of the muscle
Figure 14. A normal M-mode (unidimensional) echocardiographic image.
The left side of the diagram presents three standard directions of the ultrasonic
beam, with cardiac structures identified. The right side shows a record of
the echocardiographic images in each position as recorded on moving paper.
Abbreviations: AO, aorta; LA, left atrium; RV, right ventricle; LV, left ventricle;
IVS, interventricular septum; AML, anterior leaflet of the mitral valves; PML,
posterior leaflet of the mitral valves; LVPW, posterior wall of the left ventricle.
(Reprinted, by permission, from Arthur Selzer, Principles and Practice
of Clinical Cardiology [Philadephia: W. B. Saunders, 1983].)
of the ventricle, change in the size of the left ventricle between systole and diastole (the rate of change reflects its efficiency), the presence of fluid between the two layers of the pericardium, and the presence of abnormal structures (clots, tumors) within the cavities of the heart.
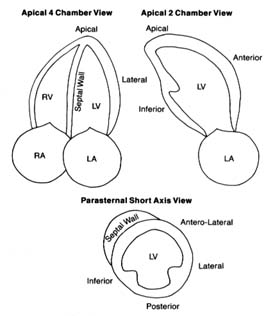
In the late 1970s a new technology was developed in the field of echocardiography permitting two-dimensional imaging. Instead of sending a single ultrasonic beam, the transducer now sends an oscillating series of beams along a single plane shaped like a large
Figure 15. The three standard views of two-dimensional echocardiographic images.
The various structures are identified, including five segments of the left ventricular
walls. The images are recorded on a videotape, which permits viewing cardiac structure
in real-time motion. Abbreviations: LV, left ventricle; LA, left atrium; RV, right ventricle;
RA, right atrium. (Reprinted, by permission, from Arthur Selzer, Principles and
Practice of Clinical Cardiology [Philadelphia: W. B. Saunders, 1983].)
slice of pie (60° to 90° of a circle). The information obtained from these echoes is processed by computer, then displayed on an oscilloscope and recorded on videotape. This technique has widened the application of echocardiography by displaying details of the interior of the heart and its various parts in motion in real time (fig. 15). It allows the cardiologist to detect abnormalities in the size, shape, and mode of contraction of each cardiac chamber, in the contraction of specific portions of the ventricular muscle, and in the thickness of cardiac valves and the size of their opening. It also can reveal
clots, vegetations, or tumors inside the heart and aid in the diagnosis of certain congenital abnormalities of the heart.
Further technological advances have applied the Doppler effect to echocardiography as a means of studying blood flow through the heart. This physical principle describes the effect of motion on sound waves: a person listening to a sound will perceive a rise in pitch if the source of the sound is approaching and a fall in pitch if the source is receding. In echocardiography the Doppler effect lets us measure the velocity of blood flow toward or away from the transducer. On the videotape these changes in velocity and direction of blood flow are displayed as variations in color. Doppler echocardiography can show the presence and approximate volume of backflow through incompetent heart valves. It also aids in evaluating shunts through abnormal communications within the heart in some types of congenital heart disease and in gauging the severity of stenosis (narrowing) of a cardiac valve as well as approximate pressures in certain parts of the heart and great vessels. Doppler echocardiography has introduced an entirely new approach to noninvasive diagnosis: whereas conventional echocardiography opened up the field of noninvasive diagnosis of structural abnormalities of the heart, Doppler echocardiography has made it possible to evaluate the dynamics of blood flow through the heart.
Another echocardiographic technique is transesophageal echocardiography , in which the transducer is placed at the end of a tube similar to that used in endoscopic examination of the stomach and esophagus. This tube is swallowed by the patient, and the transducer is lowered to the level of the heart. Since the esophagus lies immediately behind the heart, the beam does not have to pass through outer structures of the chest. Transesophageal echocardiography is thus capable of displaying images in much greater detail than conventional echocardiography. The procedure has its disadvantages, however; it cannot properly be considered noninvasive, and it causes the patient some discomfort. This technique is sometimes used to monitor the heart and its responses during certain open-heart operations. Its value in diagnostic work has not yet been completely defined, but at present it is used to evaluate some special problems when conventional techniques are inconclusive.
Echocardiography has radically altered the approach to diagnosing
heart disease. However, it is a very expensive test; hence it is used to evaluate specific problems and is not included in a routine examination. Many problems previously requiring complex invasive tests can now be adequately reviewed by echocardiography.
Other diagnostic tools involve injecting radioactive substances into the bloodstream. Such testing is the responsibility of a separate medical specialty, nuclear medicine . Although the field got its start in the 1920s, the primary application of nuclear techniques to heart disease was in research until the 1970s, when diagnostic tests were developed. Today nuclear cardiology is used extensively in diagnosis as well as research. Two important tests are myocardial isotopic perfusion imaging , in connection with exercise or pharmacological stress tests, and nuclear ventriculography , a method of studying the contraction and relaxation of the ventricles.
Perfusion tracer agents such as thallium-201 or Technetium 99m Sestamibi are injected into the bloodstream and enter the heart muscle along with the coronary blood flow. The radioactivity disappears within a few days. Their presence in the heart muscle can be detected by a special camera. Thus, if a portion of the heart muscle is receiving less blood or is totally deprived of blood, it will show in the photographs as an area of lighter contrast or as a blank space.
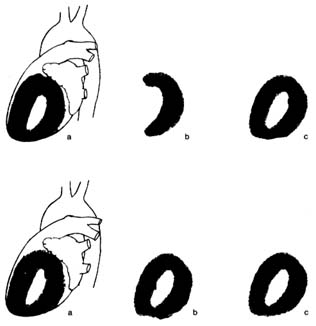
The myocardial stress perfusion test discriminates between areas of the heart muscle permanently deprived of blood supply and those rendered temporarily ischemic (fig. 16). It is usually performed in connection with a treadmill test. Just before the end of the exercise, the liquid containing the thallium isotope is injected into the bloodstream. It may be performed by using a drug stress, such as diphridamole or adenosine, in patients who are unable to do a treadmill stress test. A symmetrical, full distribution of radioactive isotopes indicates good blood supply to the heart. If an area of abnormally reduced flow is found, another count is performed four hours later (occasionally a third count is taken 24 hours later). If the defect in the image remains unchanged, the physician can conclude that the area is permanently deprived of blood flow, probably a scar from a previous myocardial infarction. If, however, the abnormality has disappeared, the proper diagnosis is ischemia, temporary blockage of blood supply, usually owing to significant coronary-artery disease.
Figure 16. Thallium perfusion scintigram (image of thallium content of the
heart used in thallium treadmill stress tests). The upper row shows a test
positive for myocardial ischemia; the lower row shows results of such a test in a
healthy person. (a) Lateral thallium image of the left ventricle superimposed on
the heart. (b) Thallium images taken immediately after exercise. The upper
drawing shows a large defect (absence of blood flow) of the anterior wall of the
heart. The lower drawing shows normal perfusion. (c) Thallium images taken
four hours after the exercise test, showing restoration of blood flow to a normal
level. If the defect in the upper row present in b would persist in c, the test
would be interpreted as showing a scar from past myocardial infarction rather
than myocardial ischemia.
Nuclear ventriculography is a method of recording the motion of the heart chambers. The blood is made temporarily radioactive by injecting into the bloodstream an isotope with a very short half-life (a few hours). The isotope in the blood lining the cavities of the cardiac chambers permits observation, on videotape, of the heart in motion during the cardiac cycle. The function of each ventricle can be assessed from the extent of the motion of its walls. The test helps in calculating an important index of ventricular function, the ejection fraction , the ratio of the blood ejected during systole to the greatest volume of the ventricle in diastole. In addition, if the
motion of the ventricular wall is abnormal, the test can reveal whether the entire ventricle is contracting sluggishly or only some parts of it. This wall motion abnormality is central to the diagnosis of coronary-artery disease.
The field of diagnostic imaging—cardiac imaging in particular—shows rapid advances. New isotopes are being developed in radiopharmacology that may refine the diagnostic value of present methods and introduce new tests. Most of the new techniques are first applied in research; only if their value in diagnosing individual cases of heart disease is demonstrated do they become generally available. The new technologies often require complex equipment costing millions of dollars. Two imaging techniques are widely used. Computed axial tomography (CAT scan ) is an X-ray technique that allows the photographing of two-dimensional "slices" through parts of the body. The resulting image is assembled and enhanced by computer. At present, the CAT scan has little application in diagnosing abnormalities of the heart itself, but it is of value in addressing certain problems of the great vessels or the pericardium. Magnetic resonance imaging generates images of internal body structures by picking up changes in cells produced by exposure to a powerful magnet. This method, too, is limited in its application to cardiac diagnosis, though it may reveal tumors of the heart and abnormalities of the pericardium. Further developments in imaging are now being tested for research purposes, such as magnetic resonance spectroscopy and positron emission tomographic imaging, both of which may help in studying metabolic changes in the heart muscle and may lead to improvements in diagnosing special cardiac problems.
Invasive Tests
The heart is a pump that drives blood into the two great vessels and maintains adequate pressure to ensure proper blood supply throughout the body. The relationship of flow and pressure in the two circulations and their respective changes are called hemodynamics . At one time hemodynamic information could only be inferred from certain observations or extrapolated from animal measurements. A new era in cardiology arrived when hemodynamic measurements became possible in humans by means of cardiac catheterization . The technique
of introducing a catheter, or thin tube, into the heart was demonstrated in Germany in 1929, but cardiac catheterization was first put to practical use in 1941 by the French-American physiologist André Cournand, who won the Nobel Prize in 1956. Cardiac catheterization remains the basic technique of many invasive procedures for the diagnosis and treatment of heart disease.
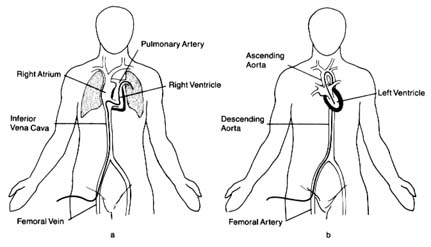
The term "cardiac catheterization" in its early days was used to mean a specific, rather limited test consisting of the introduction of a catheter into the circulation, either through a vein into the right side of the heart and the pulmonary artery or through an artery into the aorta and the left side of the heart. The catheter permitted collecting blood samples from various parts of the circulation and measuring pressures in the heart and arteries. The earliest application of cardiac catheterization was in the diagnosis of some congenital heart diseases by showing abnormal communication between the two sides of the heart and abnormal pressures in the right side of the circulation. The original method involved making an incision in the skin and directly introducing the catheter into a vein under the skin. A simplified technique, called the percutaneous method, was first introduced in Sweden. It consists of puncturing a vein with a needle through the skin and introducing a wire through the needle. The needle is then withdrawn, and the catheter is slid into the vessel over the wire. This technique is particularly valuable in catheterizing an artery, a procedure that otherwise would require minor surgery (fig. 17). Percutaneous introduction of catheters into the blood vessels is now the basis for almost all invasive procedures, not only for diagnostic purposes but also for a variety of treatments of cardiovascular conditions. The most important application of this technique is in contrast cardiovascular radiology, particularly angiocardiography.
Cardiac catheterization as a general term now applies to a combined invasive diagnostic study involving several components. The goals of cardiac catheterization as an isolated procedure include
gathering basic hemodynamic data (cardiac output, intracardiac pressures) to evaluate the function of the two ventricles with the patient at rest and during mild exercise (pedaling a stationary bicycle during the procedure)
diagnosing pulmonary hypertension
determining pressure gradients between chambers (see chap. 7), which may indicate the severity of stenosis of cardiac valves
detecting abnormal communications between the two sides of the heart
Cardiac catheterization is almost always combined with angiocardiography, considered indispensable in reaching a diagnosis.
A special application of cardiac catheterization technique is hemodynamic monitoring of seriously ill patients in intensive-care or coronary-care units. This involves introducing into a vein a small catheter with an inflatable balloon near its tip. The balloon is then inflated, and the catheter is carried by the flow of venous blood into the right atrium, the right ventricle, and the pulmonary artery. This procedure does not require a cardiac laboratory or fluoroscopic facilities and can be performed in the intensive-care unit of a
Figure 17. (a) The pathway of venous (right-sided) catheterization of the heart.
The catheter enters the body via the femoral vein in the groin and is
conducted through the inferior vena cava into the right side of the heart and
hence into the pulmonary artery. (b) The pathway of arterial (retrograde)
catheterization of the heart. The catheter is introduced into a femoral artery in
the groin and is advanced (against the flow of blood) into the aorta and through the
aortic valve into the left ventricle. The catheter can also be redirected,
above the aortic valve, to enter the origin of each coronary artery in order to
perform a coronary arteriogram.
hospital. The catheter can be left in place for several days, permitting continuous display of pressures inside the heart or pulmonary artery and intermittent determination of cardiac output.
Angiocardiography , or contrast radiography of the heart and blood vessels, is the most frequently performed study of the circulatory system and is used for examining other parts of the body as well (brain, kidney, lower extremities). It consists of introducing into the blood a liquid containing a radiopaque substance that shows up when photographed. Most tests require that the X-ray image be recorded on 35-mm film to appreciate the motion, although some tests require only still photographs. The contrast material used to be injected into the bloodstream through a vein, but it was found that the material became too dilute by the time it reached the parts of the circulation to be investigated. The standard technique now is to introduce the contrast material directly at the point of investigation by means of a catheter (selective angiocardiography ).
Coronary arteriography is the most frequently performed invasive cardiac test. Special catheters are introduced into the large artery in the groin and guided into the aorta. The performed catheter tips are conducted to the opening of each coronary artery as it leaves the aorta. A small amount of contrast material is injected directly into each, and the distribution of the opacified blood is recorded on 35-mm X-ray film. An alternate route for introducing the catheter into the arterial system is through the brachial artery (at the inside of the elbow).
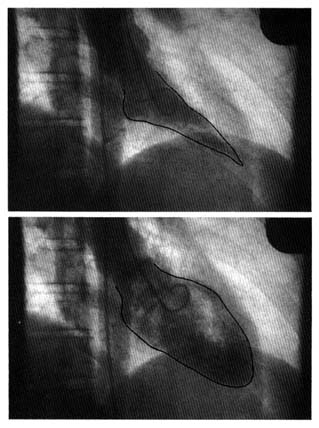
Left ventriculography is the standard procedure for evaluating contractions of the left ventricle as well as calculating the ejection fraction (fig. 18) (see the discussion of nuclear ventriculography above, pp. 39–40). In patients undergoing coronary arteriography, a ventriculography is usually performed at the same time, since the data obtained by this method are more reliable than those obtained by the noninvasive technique.
Angiocardiography plays an important role in detecting congenital heart disease. In conjunction with cardiac catheterization, it allows the physician to diagnose some of the most complex lesions. It is also essential in evaluating disease of the cardiac valves by displaying valvular incompetence.
A refinement of angiographic technique is digital subtraction angiography which enhances the faint image of opacified blood
Figure 18. Two frames from a film showing the left
ventriculogram of a healthy person, performed by
injecting a contrast dye through a cardiac catheter into
the left ventricle. The upper frame (outline retouched)
shows the volume of the left ventricle at the end of
systole (lowest volume), the lower frame at the end of
diastole (highest volume). The difference between the two
volumes represents the amount of blood ejected into the
aorta by the recorded heartbeat. The volume of ejected
blood (stroke volume) divided by the highest volume in
diastole represents the percentage of blood pumped by a
heartbeat (the ejection fraction, in this example 84
percent), an important index of cardiac performance.
when the contrast substance is too dilute to be seen under ordinary radiography. This technique permits visualization of various parts of the vascular system after the contrast material is injected into a peripheral vein. This type of angiocardiography thus becomes a noninvasive procedure (intravenous injections are considered noninvasive). It provides clear pictures of the aorta and great vessels as well as somewhat limited images of the heart. Detailed viewing, however, still requires selective angiocardiography, particularly in visualizing the coronary arteries.
Another invasive diagnostic procedure indicated in special conditions is the electrophysiological study . Wires are introduced into various areas of the heart and record electrical potential directly from the inside of the heart. Such studies may also employ stimulation of the heart by an electronic pacemaker to observe responses of the heart and induce certain arrhythmias that reproduce those experienced previously by the patient.
Diagnosing Heart Disease
Present-day technology provides many sophisticated procedures for establishing a precise and correct diagnosis in a heart patient. The process of arriving at a diagnosis involves three steps: (1) history taking and physical examination, usually supplemented by electrocardiographic and radiographic examinations, (2) complex noninvasive tests, and (3) invasive tests. In a great many cases, step 1 may establish a reasonable diagnosis. Step 2 greatly increases the cost of the diagnosis; echocardiographic and nuclear studies range from five to ten times the cost of the electrocardiogram and chest X ray. Step 3 not only raises costs still further but also introduces an element of risk—the possibility of the test causing physical complications or even death. It should be noted that noninvasive tests are performed by technicians: the physician sees and interprets only the results of the test. Echocardiography and nuclear tests thus require a great deal of expertise from the technical staff before the physician reviews the findings. Invasive tests are in essence surgical procedures performed by cardiologists with special training supported by an expert team of nurses and technicians.
Interpreting test results presents two types of difficulties. First, tests aimed at establishing the presence of a certain abnormality do
not always provide a definitive answer and may lead to a difference of opinion. Second, almost every test occasionally supplies incorrect information: certain changes expected to be present in a given disease may not be found (a false negative result), or the test may display changes suggesting a disease not present (a false positive result). In arriving at a diagnosis, the physician may encounter a maze of difficulties caused by uncertain, sometimes contradictory results of examinations and tests. Although establishing a correct diagnosis may represent a personal challenge to physicians, they should not lose sight of the goals of a detailed diagnosis: to determine the proper medical treatment for the patient and to evaluate the patient's prognosis. A diagnosis of heart disease can often involve much more testing than is necessary to fulfill these goals. Concerns about the cost of health care force us to consider the cost-benefit relationship that may lead to voluntary or imposed restrictions on performing tests, especially since cardiological procedures are among the most expensive in medicine.